A study conducted at the New York City Department of Health and Mental Hygiene, USA, and the Mailman School of Public Health, Columbia University, USA, has determined the transmission rate, immune escape ability, and infection fatality rate of the B.1.526 variant of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The findings reveal that the variant has considerably higher transmissibility and immune escape potential than previously circulating variants and that it can increase the infection fatality rate by 62% - 82% among older adults. The study is currently available on the medRxiv* preprint server.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Background
With the progression of the coronavirus disease 2019 (COVID-19) pandemic, several new variants of SARS-CoV-2 have been identified. Because of increased infectivity and pathogenicity, some of these variants have been designated as Variants of Concern (VOC) or Variants of Interest (VOI) by the World Health Organization (WHO).
The B.1.526 variant of SARS-CoV-2, also known as the lota variant, was first identified in New York City in November 2020. Later, the variant has been detected in all 52 states and other jurisdictions in the United States, as well as in 27 countries across the world.
As observed in a laboratory-based study, this variant is modestly resistant to neutralization by therapeutic monoclonal antibodies and vaccine/infection-induced antibodies. In contrast, evidence indicates that the variant does not increase the risk of breakthrough infections in vaccinated or previously infected individuals.
In the current study, the scientists have analyzed multiple epidemiological and population datasets collected in New York City and performed mathematical modeling to determine the transmission rate, immune evasion ability, and infection fatality risk of the B.1.526 variant.
Study design
The scientists utilized a network model-inference system to estimate the transmission dynamics of SARS-CoV-2 and population-level variables and parameters in New York City. Based on collected information, they conducted a city-level multi-variant, age-structured modeling analysis to estimate the infection and immune evasion ability changes for the B.1.526 variant. The final analysis utilized the data obtained from two models to estimate the variant-specific mortality rate among individuals infected with SARS-CoV-2 (infection fatality risk).
For the network model-inference system, they utilized multiple epidemiological datasets as well as vaccination datasets. Similarly, the multi-variant model analysis utilized four weekly datasets, including confirmed and suspected COVID-19 cases, hospitalizations, mortality, and percentage of different SARS-CoV-2 variants circulating in New York City.
Important observations
In New York City, the population-level prevalence of SARS-CoV-2 infection was estimated to be 16.6% at the end of the first pandemic wave. Similarly, at the end of the second wave, the estimated prevalence was 41.7%. While most infections occurred in the older population during the first wave, the second wave caused infections in all age groups.
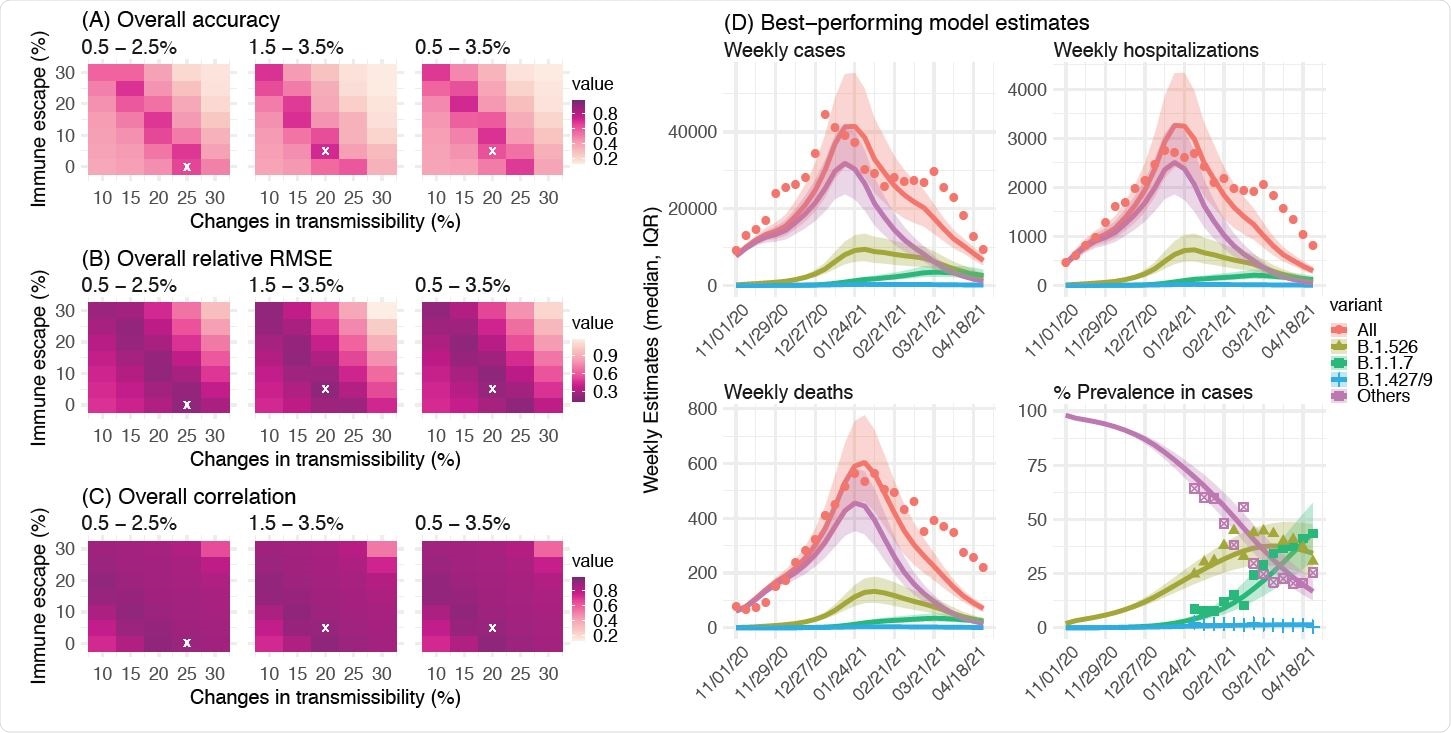
Comparison of different combinations of changes in transmissibility and immune escape property for B.1.526. Left panel shows the overall accuracy (A), relative RMSE (B), and correlation (C) of model estimates under different transmissibility and immune escape settings. White crosses (x) indicate the best-performing parameter combination. Right panel shows model estimates using the overall best-performing parameter combination (i.e., 1.5-3.5% initial prevalence, 15-25% higher transmissibility, and 0-10% immune escape). Lines and surrounding areas show model-simulated median estimates and interquartile range; dots show corresponding observations; colors indicate different variants as specified in the legend. Note that these model simulations used same infection-detection rate, hospitalization-rate and IFR (i.e., average during Nov 2020 – Apr 2021); that is, they did not account for changes in case ascertainment or disease severity by week during this period, due to, e.g., increases in disease severity by the new variants. As such, there were larger deviations from the observations during later months of the simulation with more infections by the new variants.
Transmissibility and immune evasion potency of B.1.526 variant
A rapid increase in B.1.526-infected cases was observed during the second pandemic wave. Before the identification of the variant in a specific neighborhood for the first time in early November 2020, a gradual increase in the overall SARS-CoV-2 transmission rate was observed in the same neighborhood. The transmission rate remained high between November 2020 and February 2021, followed by a reduction to the baseline when the B.1.526 variant became dominant across the city. In contrast, the transmission rate remained constant in other neighborhoods. Overall, these observations indicate that the rise in transmission rate in that particular neighborhood is probably due to the early rapid spread of the B.1.526 variant.
The estimation made from the collected data revealed that the transmission rate of the B.1.526 variant is 15 – 25% higher than that of previously circulating variants. Moreover, the data revealed that the variant can induce breakthrough infections in 0 – 10% of the population. With this moderate increase in transmissibility and immune evasion ability, the B.1.526 variant became dominant in New York City from November 2020 to March 2021. Afterward, with the surge of more infectious variant B.1.1.7, the prevalence of B.1.526 variant decreased gradually.
Infection fatality risk
Despite a reduction in mortality rate following mass vaccination, an induction in infection fatality rate was estimated in New York City during the second pandemic wave. The estimations made by the scientists about variant-specific infection and mortality rates revealed that the B.1.526 variant increases the infection fatality rates by 46%, 82%, and 62% in individuals aged 45 – 64 years, 65 – 74 years, and above 75 years, respectively. Compared to previously circulating variants, the B.1.526 variant, overall, caused a 60% induction in the infection fatality rate. This induction was comparable to that estimated for the B.1.1.7 variant.
Study significance
The study highlights the importance of monitoring the epidemiological characteristics of novel SARS-CoV-2 variants to better manage the COVID-19 pandemic.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Yang W. 2021. Epidemiological characteristics of the B.1.526 SARS-CoV-2 variant, bioRxiv, https://doi.org/10.1101/2021.08.04.21261596, https://www.medrxiv.org/content/10.1101/2021.08.04.21261596v1
- Peer reviewed and published scientific report.
Yang, Wan, Sharon K. Greene, Eric R. Peterson, Wenhui Li, Robert Mathes, Laura Graf, Ramona Lall, Scott Hughes, Jade Wang, and Anne Fine. 2022. “Epidemiological Characteristics of the B.1.526 SARS-CoV-2 Variant.” Science Advances 8 (4). https://doi.org/10.1126/sciadv.abm0300. https://www.science.org/doi/10.1126/sciadv.abm0300.