In a study conducted at Cardiff University and the University of Bristol, UK, scientists have observed that in England, the all-cause child mortality rate has dropped significantly during the first year of coronavirus disease 2019 (COVID-19) pandemic compared to that in the pre-pandemic year. The highest reduction in mortality rate has been observed in children under the age of 10 years. The study is currently available on the medRxiv* preprint server.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Background
According to a report published by the National Statistics Department, England, there is a 14% increase in population-level mortality rate in 2020 compared to previous years. A significant proportion of this excess mortality is directly associated with COVID-19 related deaths. However, several other pandemic-related factors, including saturation of critical healthcare facilities, inaccessibility to essential healthcare supports, financial insecurity, and emotional distress, may also have potential impacts.
In contrast to the population mortality rate, an overall reduction in child mortality has been observed across England. However, although susceptibility to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and severe COVID-19 is considerably low in children, there is an increasing concern over the impact of social restrictions and school closure on their mental health.
In the current study, the scientists have estimated the relative risk of child mortality across England during the first year of the COVID-19 pandemic compared to previous years.
Study design
The scientists accessed the National Child Mortality Database to collect death reports of all children who died in England between April 2019 and March 2021. To estimate the all-cause mortality rate in the pre-pandemic year and during the first year of pandemic, they have categorized collected death reports based on two time periods: April 2019 – March 2020 (pre-pandemic) and April 2020 – March 2021 (during the pandemic).
For each death case, they analyzed multiple causative factors, including suicide, substance abuse, trauma, cancer, pre-existing medical conditions, intrapartum events, premature birth, infection, and sudden unexpected death in children.
Moreover, they gathered information about the gender and ethnicity of the deceased child, age at death, place of death, and the level of deprivation.
Important observations
During the entire study period, a total of 6,490 child deaths were reported to the National Child Mortality Database. Of all deaths, 3423 occurred during the pre-pandemic year (2019 – 2020) and 3,067 occurred during the first year of the COVID-19 pandemic (2020 – 2021). This indicates a significant reduction in the total number of deaths during pandemic compared to that in the previous year.
Throughout the study period, only 70 deaths occurred following a SARS-CoV-2-positive test. Although most of the tested parameters remained similar in two time periods, the number of deaths that occurred at home was significantly higher during the pandemic year.
Furthermore, the study revealed that the reduction in child mortality significant varies with age. By considering the age at death, comparatively lower mortality of children under the age of 10 was observed in the pandemic compared to that in the previous year. Similarly, considering the month of death, the number of deaths was relatively higher in October, November, and December 2019.
Importantly, the analysis considering the reason for death revealed that the number of deaths related to infection or other pre-existing medical conditions was significantly lower during the pandemic than in the pre-pandemic period. A similar trend was also observed for deaths caused by substance abuse.
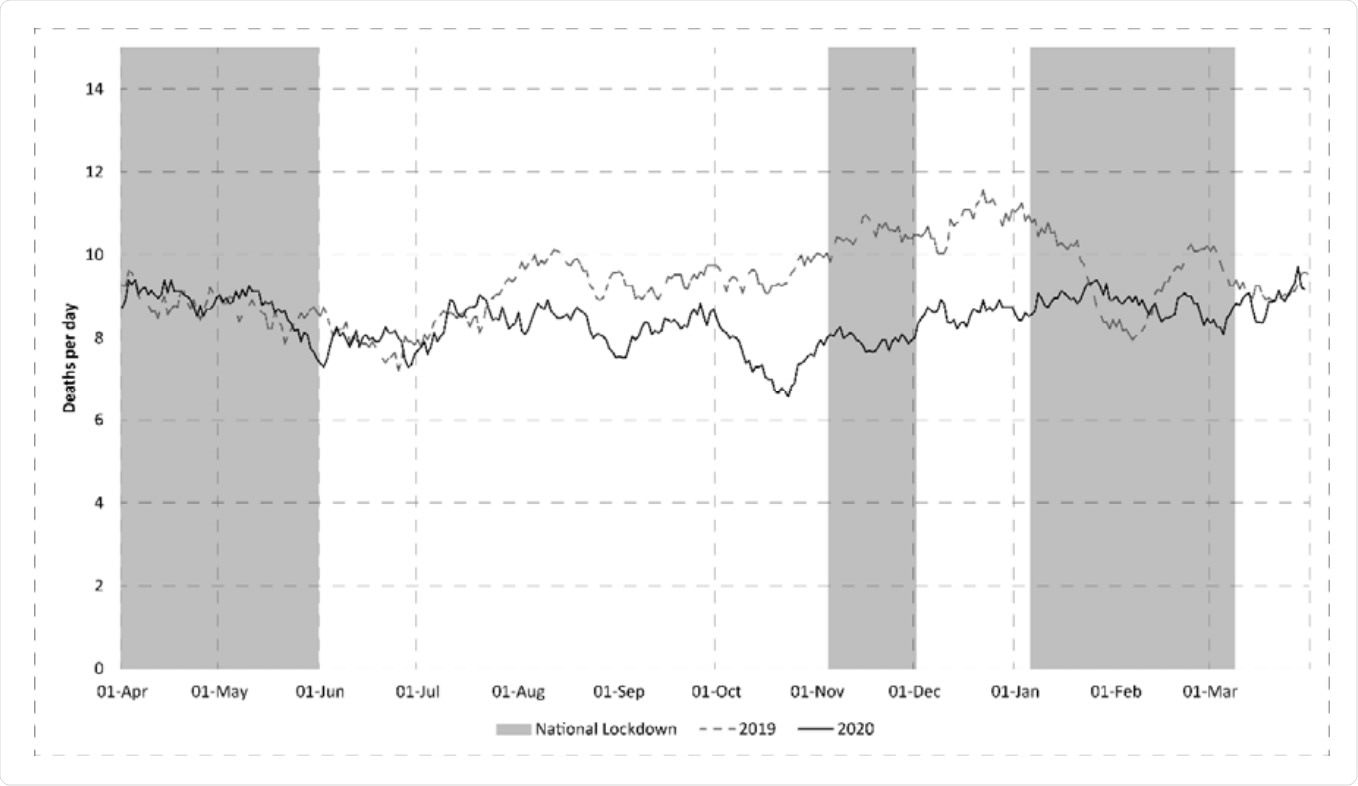
Mean Number of Deaths per day (21 day smoothed (arithmetic) average) split by time period. Periods of National Lockdown Shaded.
Study significance
Overall, the study findings reveal that all-cause child mortality in England drops significantly (around 10%) during the initial phase of the COVID-19 pandemic compared to pre-pandemic mortality. This reduction is more pronounced in children under the age of 10 years and those with infections or pre-existing medical conditions. Importantly, a similar decline has been observed in children living in the most deprived conditions.
As mentioned by the scientists, this reduced mortality could be due to a lack of exposure to seasonal viruses, including influenza virus and respiratory syncytial virus. This change in exposure pattern may impact the clinical course of otherwise common infections in upcoming years when the exposure will be higher. This, in turn, can change the rate of infection-related morbidity and mortality in vulnerable children.
Thus, more studies are required to identify the factors responsible for a reduction in child mortality.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Odd DE. 2021. Child Mortality in England During the First Year of the COVID-19 Pandemic, medRxiv, https://doi.org/10.1101/2021.08.23.21262114, https://www.medrxiv.org/content/10.1101/2021.08.23.21262114v1
- Peer reviewed and published scientific report.
Odd, David, Sylvia Stoianova, Tom Williams, Peter Fleming, and Karen Luyt. 2021. “Child Mortality in England during the First Year of the COVID-19 Pandemic.” Archives of Disease in Childhood, December, archdischild-2021-323370. https://doi.org/10.1136/archdischild-2021-323370. https://adc.bmj.com/content/107/3/e22.