Like many US states, Texas introduced many different measures to reduce the transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), such as masking, social distancing, and the closure of public services and businesses likely to aid the spread of disease.
These proved effective not only against SARS-CoV-2 but a wide variety of other respiratory diseases such as influenza viruses, rhinovirus, enterovirus and respiratory syncytial virus (RSV).
When some of the earliest disease-control restrictions were lifted, cases of SARS-CoV-2 rose steadily, but alternative respiratory infections initially remained low.
Researchers from the Houston Methodist Research Institute and Houston Methodist Hospital investigated the rate at which these diseases returned. The results were published ahead of print in the journal Microbiology Spectrum alongside a stark warning.
Early efforts to hinder the spread of SARS-CoV-2 in Houston began with canceling some large gatherings such as the Houston Livestock Show and Rodeo on the 11th of March 2020. By the 25th, the entire city was under a stay-at-home order which closed all businesses that were not essential, banned residents from leaving their home for any reason other than essential activities (such as buying groceries and exercising), and enforced social distancing.
Further restrictions included the expansion of mayoral powers to prevent outdoor gatherings, executive orders requiring masks over the face and nose in counties with over 20 positive COVID-19 cases, and travel restrictions.
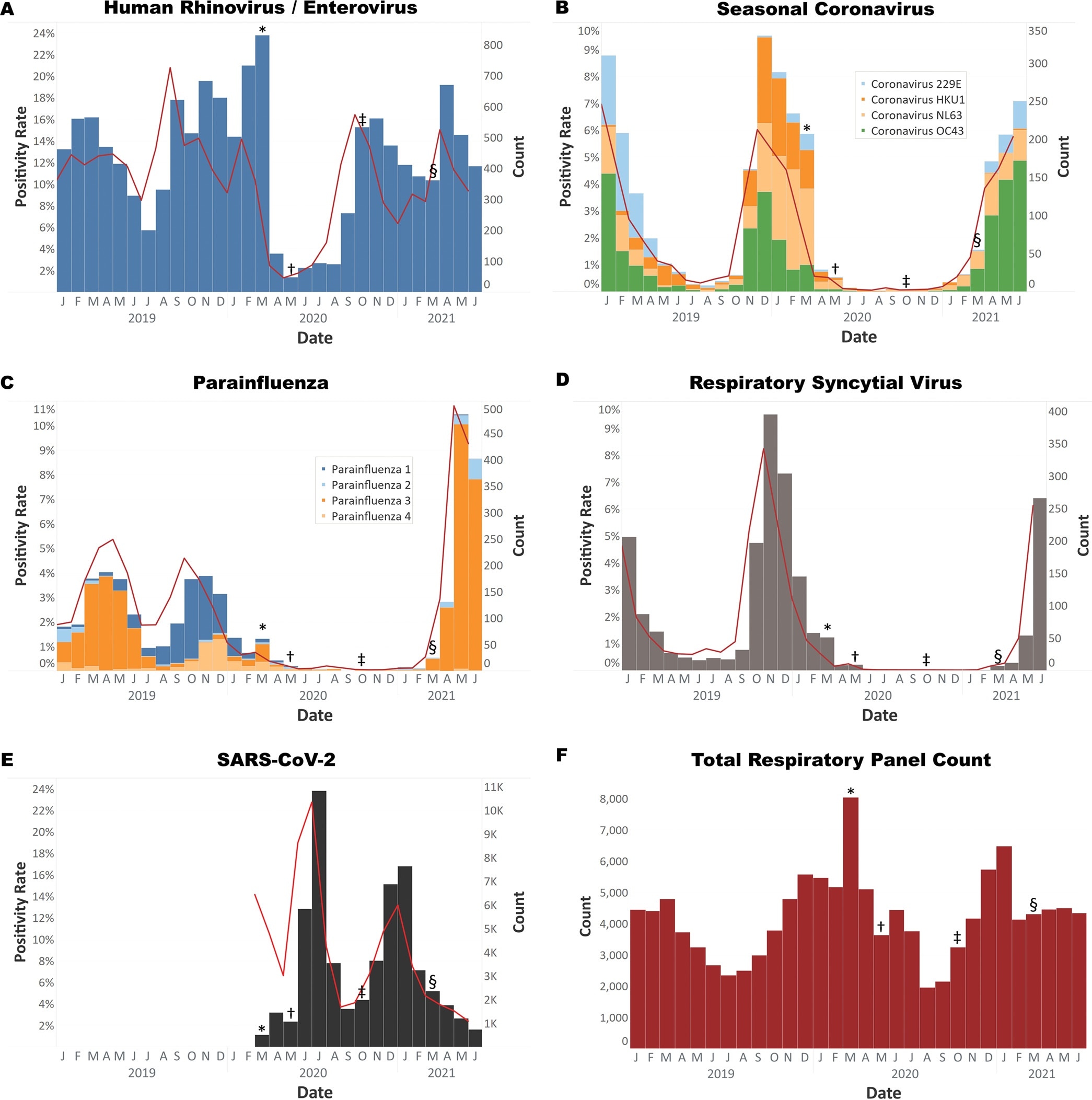
Histograms of respiratory virus tests from 1 January 2019 to 25 May 2021. (A) Rhinovirus/enterovirus was the first virus to rebound to prepandemic levels. (B) Coronaviruses 229E, HKU1, NL63, and OC43. OC43 has been prevalent since March 2021. (C) Parainfluenza viruses 1 to 4. Parainfluenza 3 has been prevalent since March 2021. (D) Respiratory syncytial virus has also increased in prevalence since March 2021. (E) SARS-CoV-2 testing volume and positivity from March 2020 through June 2021. (F) Respiratory panel test volume from January 2020 through June 2021. Symbols indicate the implementation and relaxation of COVID-19 precautions. *, March 2020, start of pandemic lockdown measures; †, May 2020, phase one reopening of Texas; ‡, October 2020, additional reopening measures; §, March 2021, removal of all COVID restrictions, including elimination of mask mandates. All tests were performed on the Biofire respiratory pathogen panel, with the exception of (E) which represents all SARS-CoV-2 PCR testing performed using multiple test vendors.
These measures were found to be highly effective in inhibiting the circulating levels of the SARS-CoV-2 pathogen. Shortly after these restrictions were implemented, the respiratory pathogen panel in Houston Methodist Hospital showed rapidly declining levels of other respiratory viruses.
Unfortunately, when the measures were removed, SARS-CoV-2 transmission did not remain low for long. From May 2020 to September 2020, most disease-controlling measures remained in place, and the Houston Methodist Hospital saw less than 5 cases of disease caused by influenza viruses per week, with even lower levels of RSV.
Rhino/enterovirus cases also remained low, with under 30 cases a week. In September, schools in Texas reopened, and the instances of rhino/enterovirus began to rise.
The speed at which infections spread rose to over 150 cases a week when measures were further relaxed in October 2020. In March 2021, all remaining measures were removed, including an obligation to wear masks in public places.
The monthly cases of seasonal coronaviruses such as those that cause the common cold rose from >50 in February to over 150 by April, rhinovirus, and enterovirus showed an increase of 300 cases in April, but both parainfluenza and RSV infection showed the most dramatic increases, with parainfluenza rising from nearly zero cases to almost 500, and the similarly low numbers shown by RSV rose to 250 cases in June.
Typically these diseases show the most transmission during winter, and a peak of cases in summer is an oddity. The authors worry that out-of-season infections could have dangerous consequences.
As these diseases are not generally seen at this time, physicians could misdiagnose patients with COVID-19, as some of the alternate infections show very similar symptoms.
Even worse, if cases of seasonal respiratory viruses continue to rise, they could overwhelm hospitals and take up beds - which could be catastrophic during the ongoing COVID-19 pandemic.
The scientists highlight the need for measures such as social distancing and wearing masks to reduce the likelihood of transmission of respiratory diseases.