The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has taken an enormous toll on the human race, as it has caused the deaths of over 4.69 million and infected almost 229 million worldwide. A new study published on the preprint server medRxiv* finds that hypertension following the viral infection is associated with a high placental viral load in pregnant women who are diagnosed with the coronavirus disease 2019 (COVID-19).
Pregnancy has been identified as a high-risk condition for severe COVID-19. In fact, preterm delivery, hypertensive disorders of pregnancy, and miscarriage have been linked to the occurrence of COVID-19 in pregnancy.
In the current study, the researchers found that SARS-CoV-2 is present much more often in the placenta of women who suffer COVID-19 during pregnancy and subsequently develop hypertensive disorders of pregnancy (HDP). Among these is pre-eclampsia, which is characterized by its occurrence only during pregnancy and by the endothelial abnormalities induced by the virus that causes multi-organ dysfunction.
COVID-19 is itself associated with endothelial inflammation in different organs that are induced both by the virus and by the inflammatory response of the host. The angiotensin-converting enzyme 2 (ACE2) receptor, which is used by SARS-CoV-2 to gain entry into the host, is expressed in the lung alveolar epithelium, as well as in the endothelial cells, which may be vulnerable to direct viral attack.
The dysregulated release of cytokines may also fuel the endothelial damage. Taken together, these factors lead to the vascular damage and inflammation caused by endothelial injury. This type of injury can result in thrombosis and micro-angiopathy, all of which are related to underlying endothelial dysfunction.
The reasons for COVID-19-like pre-eclampsia are unknown; however, some think that it may be due to the presence of the virus in the placenta. This was initially thought to be an infrequent event, bolstered by the rare occurrence of vertical transmission from SARS-CoV-2-positive mothers during the last few weeks of pregnancy.
Recently, researchers showed that SARS-CoV-2 was present at low levels in approximately 50% of placentas. However, no signs of injury or any correlation with poor outcomes in the mother or the fetus were reported.
High levels of viral ribonucleic acid (RNA) were found in a single patient who also had a serious injury to the placenta, as demonstrated by widespread fibrin deposition, necrosis of the nutritive layer, and cell death. This prompted the current study, which aimed to examine how the viral load in placental tissue at the time of birth was related to the development of HDP.
About the study
In the current study, the scientists found that of 14 women with COVID-19 and HDP, 9 women had pre-eclampsia, while the remaining 5 had gestational hypertension. As compared to control COVID-19-positive pregnancies, the HDP-COVID-19 cohort had lighter babies at about 2.9 kg versus 3.2 kg in the former group. This may be due to the larger number of women who were induced for labor or had Cesarean section in the HDP group.
However, the proportion of babies who were small for gestational age (SGA) or acidotic were similar in both groups. Only two of the 28 women in the two cohorts had severe symptoms, with 13 each reporting no or mild symptoms.
The number of placentas with SARS-CoV-2 RNA was 10, with nine of these being in the HDP group and 7/9 being in women with pre-eclampsia. Three of the RNA-positive placentas showed high RNA loads, with the cycle threshold being 28 or less as compared to a median of 30.6 in the seven remaining placentas.
All six women with HDP had RNA-positive placentas, and all had been infected during the first or second trimester. In contrast, one of the six controls infected at the corresponding stage but without HDP tested positive for placental SARS-CoV-2 RNA. There is a chance that the presence of the virus promotes HDP, or that HDP encourages SARS-CoV-2 to colonize the placenta.
Of the 10 pregnancies with early infection, one remained positive until delivery, whereas seven placentas showed the presence of the virus. Early infection in pregnancy appears to predispose the persistence of SARS-CoV-2 in the placenta.
While 13 babies were positive for antibodies to the virus within their first ten days, all showed the presence of immunoglobulin G (IgG), an antibody class that typically represents a later stage of the immune response. The acute-phase antibody, IgM, was not found in any of the ten babies. IgA, which is also related to the early phase of the immune response, was also not detected in any of the ten babies.
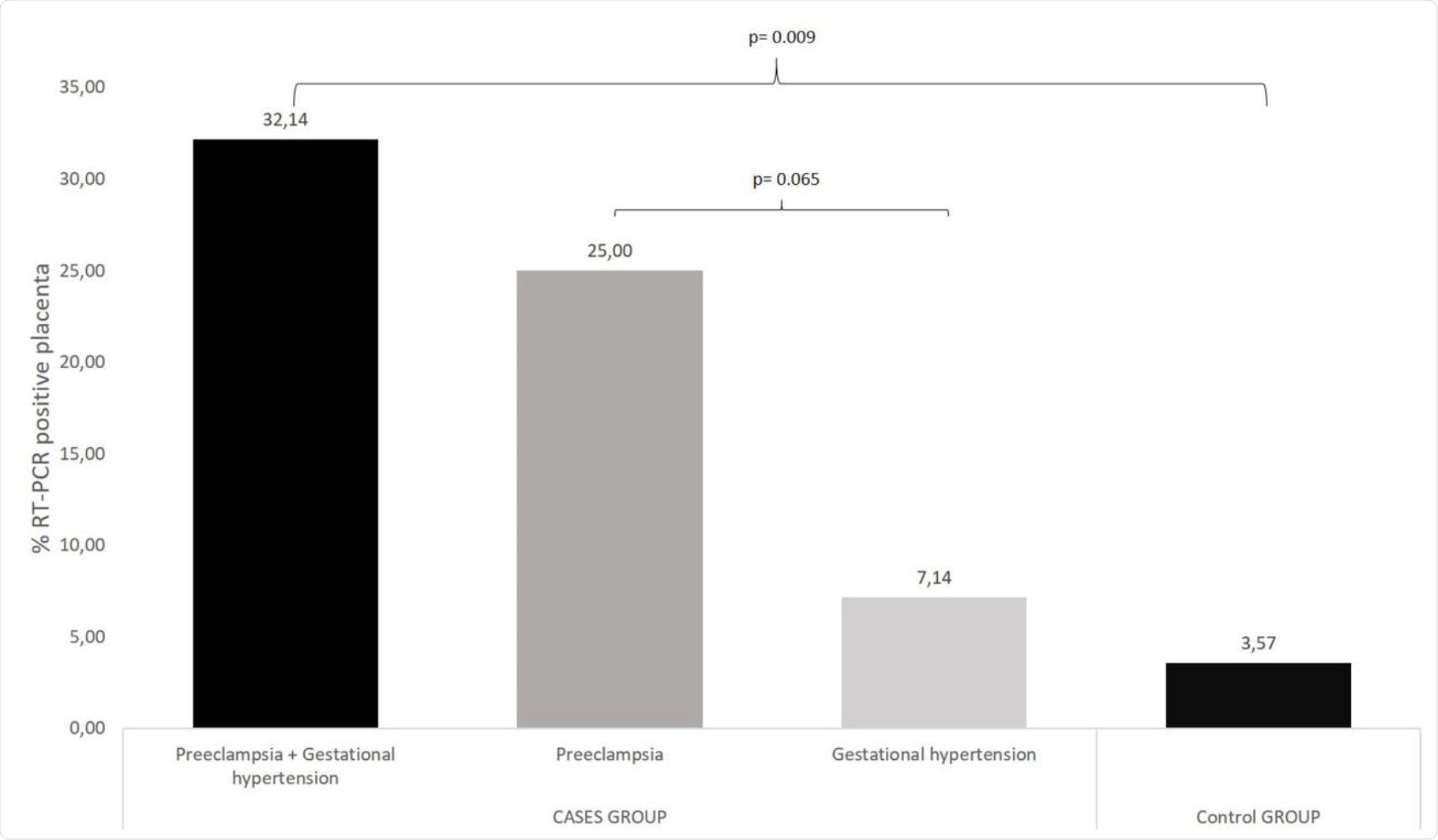 % RT-PCR positive placenta: cases group vs control group. Ten placentas (35.7% = 3.57% + 32.14%) tested positive for SARS-CoV-2 RNA. Nine positive placentas in the cases group (9/28, 32.14%) while in control group only one placenta were positive (1/28, 3.57%). Seven (7/28, 25%) belong to women diagnosed with preeclampsia vs two of nine belong to women diagnosed with gestational hypertension (2/28, 7.14%).
% RT-PCR positive placenta: cases group vs control group. Ten placentas (35.7% = 3.57% + 32.14%) tested positive for SARS-CoV-2 RNA. Nine positive placentas in the cases group (9/28, 32.14%) while in control group only one placenta were positive (1/28, 3.57%). Seven (7/28, 25%) belong to women diagnosed with preeclampsia vs two of nine belong to women diagnosed with gestational hypertension (2/28, 7.14%).
The three placentas with high viral loads were from women with severe pre-eclampsia. The authors briefly discussed the three cases, of which one was infected early with the virus, testing negative after two weeks. This patient developed pre-eclampsia at 35 weeks, was hospitalized and the baby delivered two days later weighing 1.9 kg. This woman was negative for the virus at admission, and the baby was seronegative.
The second woman had a twin pregnancy and contracted the virus at almost 27 weeks, with a very high viral load, and tested negative at 34 weeks. Her two babies were delivered by emergency Cesarean section at 37 weeks because of pre-eclampsia, which presented at week 35 but was non-severe until week 37. The twin babies weighed 3.3 and 3.4 kg, respectively, and cord blood was IgG-positive and IgM-negative.
The third woman also had a twin pregnancy, with a low risk of early-onset pre-eclampsia. She tested positive for the virus at 38 weeks with hypertension. The onset of HELLP syndrome at 38 weeks led to an elective Cesarean section, with the babies weighing 2.8 kg each. Both babies tested positive for SARS-CoV-2 and seroconverted during their third week after birth. The placenta also tested positive for the virus.
Implications
The findings of this study show that pregnant women with COVID-19 who develop HDP are much more likely to have detectable virus in the placental tissue as compared to those without HDP. Secondly, pre-eclampsia is linked to a higher viral load in the placenta than gestational hypertension.
In the above cases, the infection occurred in the first, second, and third trimesters, respectively.
“A relationship between a higher viral load in placenta tissue and the severity of the hypertensive disorder deserves consideration.”
Further research involving a larger number of patients will be required to confirm such a link, as well as the mechanism if present. Suggested pathogenetic mechanisms include endothelial injury due to infection, host inflammatory response, or infection of the nutritive cells of the placenta.
“Our work contributes to the understanding of how SARS-CoV-2 virus affects pregnancy. Better understanding of the placental disease process may aid or could be essential for appropriate monitoring during pregnancy and providing appropriate postnatal care.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Fabre, M., Calvo, P., Ruiz-Martinez, S., et al. (2021). High Viral SARS-Cov-2 Load In Placenta Of Patients With Hypertensive Disorders After COVID-19 During Pregnancy. medRxiv. doi:10.1101/2021.09.07.21261607. https://www.medrxiv.org/content/10.1101/2021.09.07.21261607v1
- Peer reviewed and published scientific report.
Fabre, Marta, Pilar Calvo, Sara Ruiz-Martinez, Maria Peran, Daniel Oros, Ana Medel-Martinez, Mark Strunk, Rafael Benito Ruesca, Jon Schoorlemmer, and Cristina Paules. 2021. “Frequent Placental SARS-CoV-2 in Patients with COVID-19-Associated Hypertensive Disorders of Pregnancy.” Fetal Diagnosis and Therapy 48 (11-12): 801–11. https://doi.org/10.1159/000520179. https://www.karger.com/Article/FullText/520179.