The study results suggest full vaccination prevented about 95% of potential hospitalization when the Alpha and Delta variant was circulating widely. Moreover, vaccines were 97% effective in preventing ICU admission.
“Among the unvaccinated population, the incidence of COVID-19 hospitalizations and ICU admissions is high, which, combined with the size of this population, could lead to a significant strain on health care in the coming months. A further increase in vaccination coverage is key to reduce the burden on health care,” concluded the team.
As COVID-19 cases rise from the Delta variant, the results reinforce the need for vaccination in preventing severe COVID-19 infection.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Vaccination status during and after the investigation
From April 4, 2021, to August 29, 2021, the team enrolled 15,571 people hospitalized for COVID-19 infection into the study. In the Netherlands, Alpha was the dominant variant from April 4, 2021, to May 29, 2021. This position was taken over by Delta, which circulated from July 4, 2021, to August 29, 2021 — the end of the study period.
The researchers defined someone as being fully vaccinated 14 days after the second dose or 28 days after the first Johnson & Johnson dose. Partial vaccination was defined as 14 days after one vaccine dose.
Of the enrollees, only 5.7% were fully vaccinated. About 7.1% were partially vaccinated, and 87.2% were unvaccinated.
Approximately 7,406 of the 13,574 unvaccinated patients got vaccinated after being hospitalized.
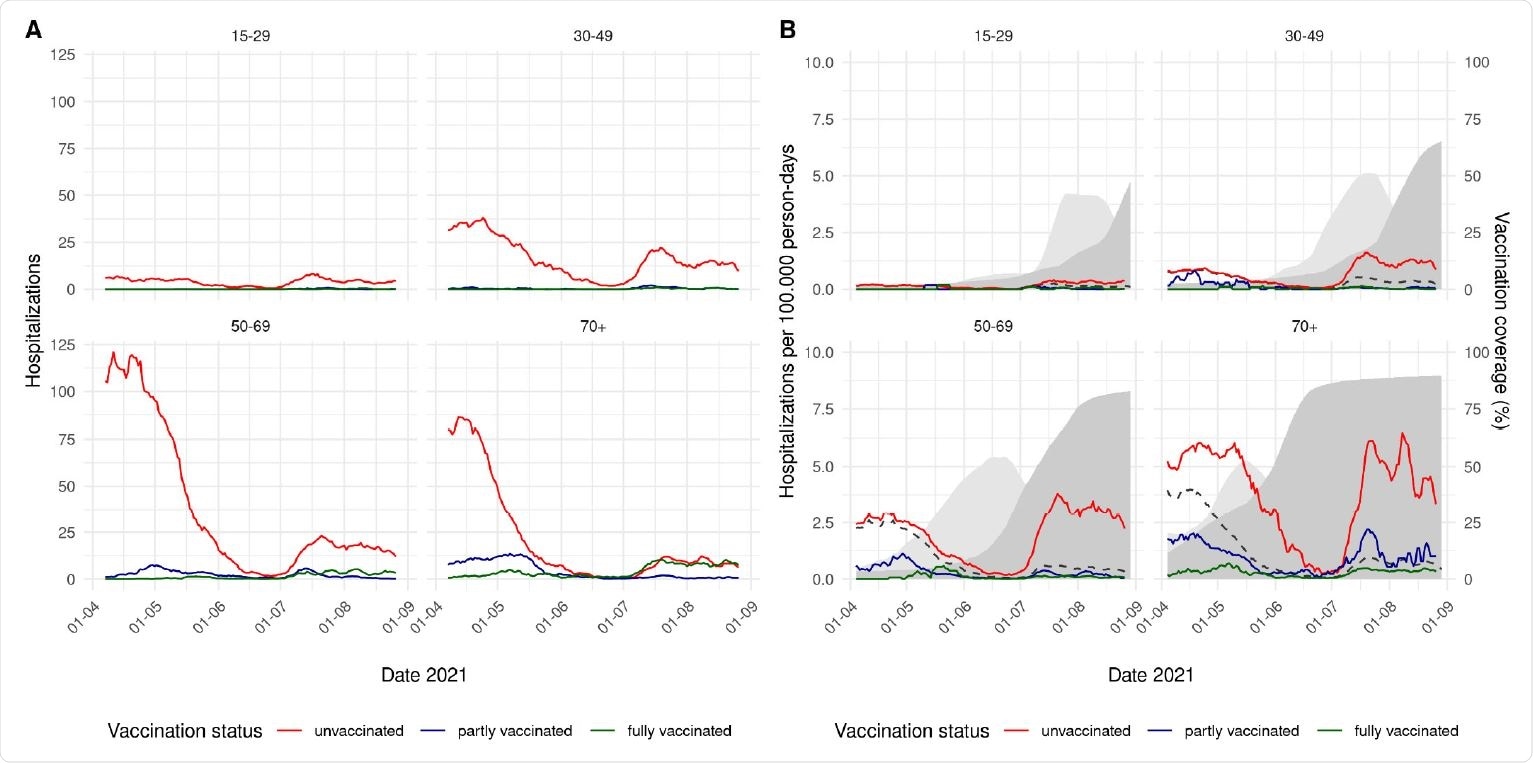
A. 7-day moving average of the number of COVID-19 hospitalizations by vaccination status and age group, 4 April – 29 August 2021. B. 7-day moving average of the incidence rate of COVID-19 hospitalizations per 100.000 person-days by vaccination status and age group, 4 April – 29 August 2021. The dashed line shows the overall incidence in the age-specific population. The light grey area shows the percentage of partly vaccinated persons in the population, the dark grey area the percentage of fully vaccinated persons.
Vaccinated people have a lower risk of hospitalization
A majority of hospitalizations were from unvaccinated patients. Results showed that the likelihood of being hospitalized is smaller among vaccinated patients compared to unvaccinated people.
When fully vaccinated, vaccine effectiveness against hospitalization was 94% when Alpha was the dominant variant. Meanwhile, vaccines were 95% effective when Delta was dominant.
Similar results were observed in the ICU as unvaccinated people made up a majority of ICU admissions. When fully vaccinated, vaccines were 93% effective in preventing ICU admissions during the Alpha period. For Delta, vaccines were 97% effective.
Only a tiny amount of the study participants was fully vaccinated, making it difficult to assess how the type of vaccine affected vaccine effectiveness. Regardless, vaccine effectiveness was high for people of all age groups and in all four vaccines — except for Moderna’s vaccine Spikevax. Although the researchers suggest the lower vaccine effectiveness from Spikevax may have been because the vaccine was primarily given to patients who were already at high risk for severe COVID-19 disease.
“Please note that in the Netherlands, persons with a medical condition putting them at high risk of severe COVID-19 were specifically given the Spikevax vaccine. The Janssen vaccine is not allocated to elderly in the Netherlands; therefore no VE for ≥70 was estimated,” explained the researchers.
Vaccine effectiveness against hospitalization and ICU admission did not appear to decrease 20 weeks after full vaccination.
Study limitations
The researchers gathered data on COVID-19 vaccination status did not include patient information on comorbidities. Having a preexisting health condition increases your risk of developing severe infection and could also explain the low vaccine effectiveness from Spikevax since it was administered in high-priority groups.
Another study limitation was how patients were enrolled in the study. The registry included patients who did not enter the hospital for COVID-19 infection but rather people who later tested positive. The researchers suggest this could cause a bias in vaccine effectiveness estimates because it affects the severity of infection in some patients. Although, they note that misclassification is more likely to occur with vaccinated patients.
Lastly, the registry used to collect patient information had incomplete data. In the Netherlands, informed consent is needed to register as vaccinated in the system. Vaccinated patients who did not provide consent may have been mislabeled as unvaccinated, leading to potential overestimation of vaccine effectiveness.
The team assumed that if 7.3% of patients were miscategorized as unvaccinated, vaccine effectiveness estimates could be reduced by 1-2%.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.