Tinnitus, although subjective, can have deleterious effects both on mental health and the quality of life of an individual. Up to 50 million adults in the United States are affected by tinnitus, with 16 million being chronic or frequent cases. While the majority of cases of tinnitus are associated with hearing loss, about 10% of the cases show no changes in hearing sensitivity.
There have been reported cases of tinnitus, vertigo, and sensorineural hearing loss occurring after individuals have recovered from the coronavirus disease 2019 (COVID-19). However, the correlation and causation are yet to be determined.
The effects of COVID-19 on neurosensory systems have not been fully comprehended. However, it has been hypothesized that COVID-19 results in neurosensory dysfunction that mostly manifests as olfactory and gustatory alterations in up to 30% of patients.
Several mechanisms for audio-vestibular disorders associated with COVID-19 have been proposed. One such hypothesis is that persistent inflammatory cytokines in the inner ear causing direct cochlear and labyrinthine injury.
Additional proposed mechanisms include a concomitant autoimmune response or the invasion of nerves by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) through angiotensin-converting 2 (ACE) receptors. The use of ototoxic drugs, such as hydroxychloroquine and macrolides, to treat COVID-19 can also cause such audiological issues to arise.
Case presentation
A 49-year-old male presented to the Mayo Clinic in Rochester, Minnesota with tinnitus. The patient had no history of tinnitus prior to this; however, his past medical history included hyperlipidemia and confirmed COVID-19 infection three months prior. Notably, the patient experienced only mild symptoms that did not require hospitalization.
Subsequently, the patient developed tinnitus that was constant throughout the day with increased severity at night. Tinnitus was bilateral, constant, and non-pulsatile. The patient described it as a “high-pitched buzzing sound.”
Normal thresholds of audiometric testing were demonstrated through 8000 Hz; however, there was mild bilateral hearing loss above 12.5 kHz. Tympanometry depicted normal tympanic membrane movement. Word recognition scores with the use of isophonemic stimuli were 100%, bilaterally.
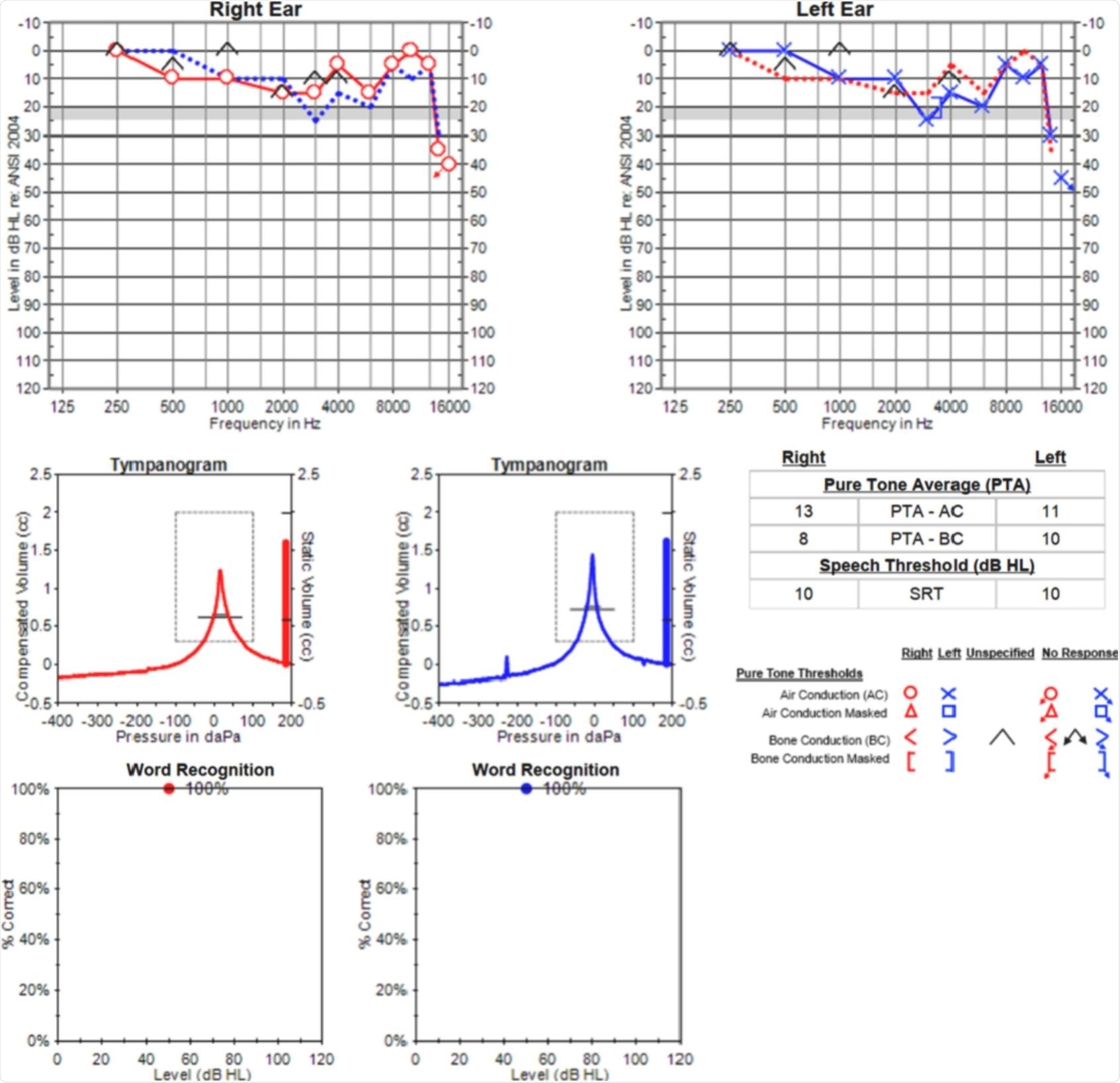 Audiometric testing revealed normal hearing thresholds through 8000 Hz, with mild bilateral hearing loss above 12.5 kHz. Tympanometry was normal, and word recognition scores were excellent bilaterally.
Audiometric testing revealed normal hearing thresholds through 8000 Hz, with mild bilateral hearing loss above 12.5 kHz. Tympanometry was normal, and word recognition scores were excellent bilaterally.
Initially, conservative measures were adopted, such as white noise masking and educating the patient. However, the patient’s tinnitus persisted and was genuinely affecting his quality of life.
The patient was then started on 300 milligrams (mg) of gabapentin daily for two weeks, which was well tolerated and further titrated to twice a day. This caused the tinnitus symptoms to improve significantly. While the patient continued to have tinnitus, the symptoms had reduced to a tolerable level, and this effect continued.
Previous research on tinnitus and COVID-19
Earlier studies have explored a correlation between COVID-19 infection and the onset of tinnitus; however, an association between the two events remains to be established by an appropriately designed study.
Current research cannot conclusively explain how patients develop severe tinnitus without associated hearing loss or mild hearing loss. Therefore, several hypotheses are worth exploring.
Psychological triggers, especially factors such as loneliness, poor quality sleep, depression, and anxiety, have been aggravated during this pandemic situation. These factors may also play a role in triggering or worsening tinnitus. Some studies have shown that symptoms of patients with pre-existing tinnitus worsened during the pandemic, regardless of their COVID-19 status.
Previous trials have attempted to establish new-onset tinnitus without new subjective hearing loss. However, these studies relied on subjective hearing data and failed to utilize objective audiometric testing results.
Another cross-sectional, multicenter study of 3,103 individuals with COVID-19 found that 54% reported no change in tinnitus, 40% reported no change in tinnitus, 6% reported improved tinnitus, and only 0.2% reported new-onset tinnitus after COVID-19 infection.
Recent studies which explore new-onset tinnitus following COVID-19 may suggest that the rates of tinnitus in patients with normal or mild hearing loss may be higher in this population. Comparatively, another study reported having detected a mild transient decline in pure tone thresholds in two patients with no subjective hearing loss, thereby suggesting no associated cochlear impairment.
Study takeaways
Usually, patients suffering from tinnitus report milder symptoms when associated with normal to mild hearing loss as compared to those with higher degrees of hearing loss. The case presentation with severe tinnitus deviates from this pattern. Here, conservative treatments were not successful and, eventually, gabapentin was found to efficiently reduce the severity of tinnitus.
Questions arising from this case presentation and other COVID-19 patients include:
- Does COVID-19 cause tinnitus?
- Is the pathophysiology of COVID -19 different from tinnitus associated with hearing loss? If so, will it have to be treated differently as a result?
A direct association between COVID-19 and new-onset tinnitus has not yet been established. In fact, this case report may be representative of a subset of patients with largely normal hearing who suffer from severe tinnitus without the loss of hearing post-COVID-19.
This association can only be established through careful data-driven analysis. Moreover, the pathophysiology of tinnitus in this subset of the population may indeed be unique; thus, the role of neuromodulators needs to be established.