The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causal agent of the coronavirus disease 2019 (COVID-19) pandemic, was first identified in Wuhan, China, in 2019. Since then, the virus has mutated, leading to the emergence of new variants of interest (VoIs) and variants of concern (VoCs).
Widespread testing has been identified as one of the ways to keep track of the spread of the virus, which could, in turn, lead to targeted measures to contain the pandemic. Twice-weekly testing has been shown to be adequate to contain the spread of the original strain from Wuhan. However, this might not be the case for the other VoCs, such as the Delta variant.
In a new study published on the medRxiv* preprint server, scientists have used available data on the Delta variant’s viral load to infer its infectiousness and, subsequently, estimate the reduction in its transmission brought about by surveillance testing. The testing, done at different frequencies, was performed on a susceptible population. The cases of both the original Wuhan strain and the Delta variant were considered.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
A New Study: Surveillance Testing
Besides symptomatic individuals, COVID-19 may be transmitted by individuals who do not show symptoms (i.e., asymptomatic or pre-symptomatic). In fact, recent data shows that asymptomatic and pre-symptomatic individuals account for 59% of the transmissions. Surveillance testing involves testing individuals at regular intervals, irrespective of whether they report symptoms or not. Individuals who test positive are isolated and close contacts are quarantined. The main goal of this protocol is to reduce community transmission by identifying and isolating early.
Surveillance testing requires a sensitive test capable of detecting small amounts of viruses and a frequent test. The latter aids in identifying infected individuals before or while they are infectious. In the current study, scientists have estimated how frequently individuals must be tested to reduce transmission.
The correct answer depends on how quickly the virus becomes active within a host and is, therefore, different for different strains of the virus. Scientists have used laboratory data and mathematical analysis to document that for the Delta variant, every other day testing may be advisable.
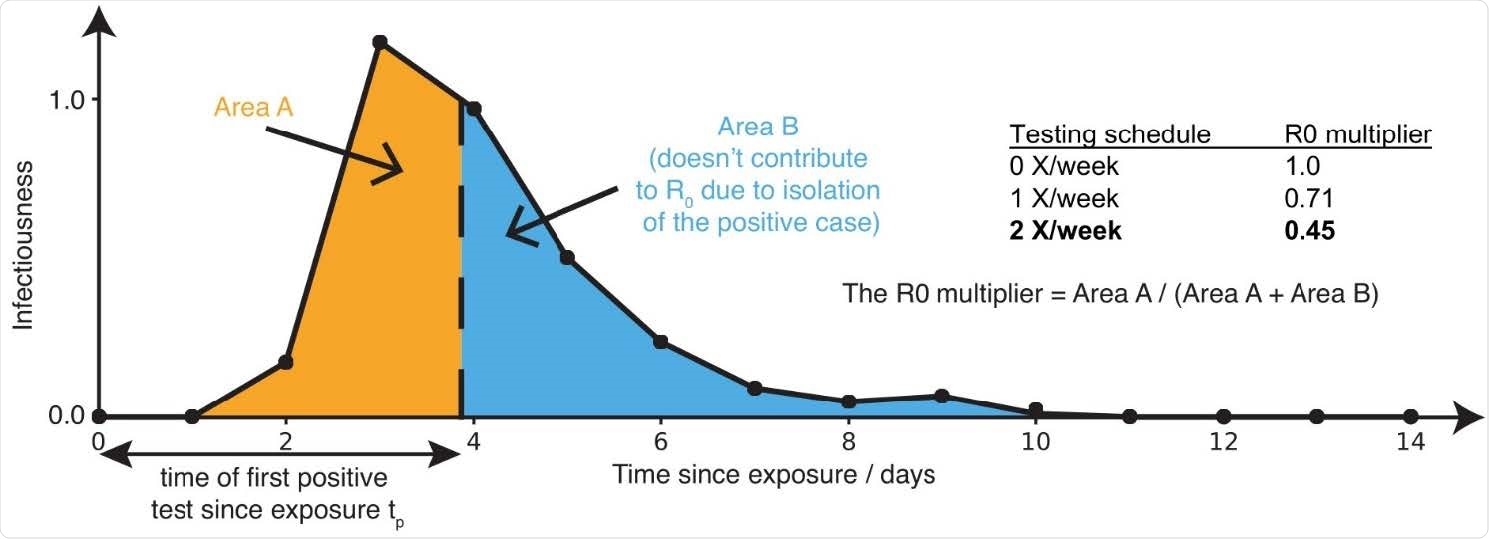
Sensitive testing can reveal a positive case early in the infection, and thus isolation of the index case reduces the number of people infected by this index case. Frequent testing and rapid isolation reduce the time period during which a person is infectious but not isolated (Area A). As a result, the R0 multiplier for testing is the ratio between the truncated area under the curve (Area A) and the untruncated area under the curve (Area A + Area B). The dashed vertical line between Area A and Area B represents the moment an infected individual is isolated; as this line moves to the left, M is decreased, and viral spread is reduced.
An Overview of the Testing Method
A SHIELD saliva test was used for this study, whose sensitivity two days prior to the start of infectivity ranges between 84% and 88%. This is much higher than nasal or antigen tests. When conducted once a week, the SHIELD saliva test has a 58% chance of detecting individuals while infectious, and this number rises to 80-85% when the test is performed twice a week. The test is also highly effective in detecting any infection at all (about 90%). When conducted twice a week, the chance of detection goes up to a very impressive 95%.
Main Findings
Scientists observed that for the original Wuhan strain of SARS-CoV-2, testing twice a week could bring down the reproduction number (R0) significantly below 1. However, for the Delta variant, limited information is available, which led the scientists to consider two different scenarios for the viral load profile. The first scenario considered the Delta viral load to be peaked and similar (qualitatively) to the original strain. In contrast, the second scenario was more data-driven in that the Delta viral load has a plateau at its peak value.
The growth rate of the viral load of the Delta variant was found to be about 4-5 orders of magnitude, compared to 2-3 orders of magnitude for the ancestral strain. This proves the significantly higher infectiousness of the Delta variant. Scientists estimated the frequency of surveillance testing to reduce the reproduction number well below 1. They found that testing every other day was much more effective than testing once or twice a week. These calculations were based on the assumption that individuals would self-isolate one day after symptoms appeared; otherwise, they would continue to transmit the virus.
Besides the increased testing frequency, the speed of returning results and quick isolation of infected individuals are also extremely crucial. Delays in any of the above are likely to hamper the efforts to contain the virus, especially given the rapid viral dynamics and high viral loads.
Conclusion
In this article, scientists have shown that testing unvaccinated individuals every other day for the Delta variant could significantly reduce transmission. It must be noted that testing alone cannot guarantee the containment of the virus. We need a much more coordinated effort; a combination of various factors, such as vaccination, masking, good ventilation, surveillance testing, and other non-pharmaceutical interventions may be required to curb the spread of the pandemic.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.