The causal agent of the ongoing coronavirus disease 2019 (COVID-19) pandemic is the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). SARS-CoV-2 was first reported in 2019 in Wuhan, China, and was characterized as a positive sense, single-stranded ribonucleic acid (RNA) virus belonging to the family Coronaviridae of the genus Betacoronavirus.
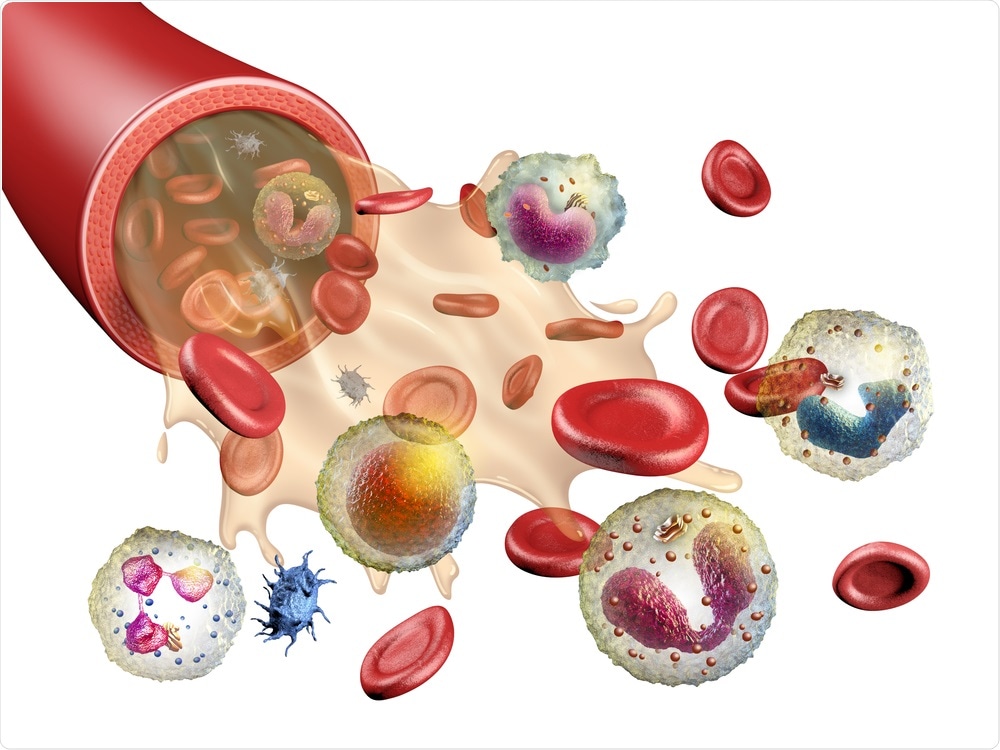 Study: CCR2 Signaling Restricts SARS-CoV-2 Infection. Image Credit: Andra Danti / Shutterstock.com
Study: CCR2 Signaling Restricts SARS-CoV-2 Infection. Image Credit: Andra Danti / Shutterstock.com
Background
The innate immune response against SARS-CoV-2 involves limited production of interferon (IFN), and inflammatory cytokines such as interleukin-6 (IL-6]), IL-1β, tumor necrosis factor-alpha (TNF-α), and IL-8 by alveolar macrophages or respiratory epithelial cells. Previous studies involving the analysis of bronchoalveolar lavage (BAL) fluids of SARS-CoV-2-infected individuals reported a correlation between the innate immune response and vigorous infiltration of neutrophils, dendritic cells (DCs), and monocytes into the lung airways.
Scientists have categorized monocytes in the lung parenchyma into subpopulations based on their expression of Ly6C. Previous studies have indicated that Ly6C-high classical monocytes are pro-inflammatory, whereas Ly6C-low non-classical monocytes are involved with healing wounds.
In homeostatic conditions, Ly6C-low monocytes are dominant. Comparatively, during acute infection, Ly6C-high monocytes infiltrate the lungs in a CCR2-dependent manner.
Earlier studies have also shown that classical Ly6C-high monocytes can differentiate into monocyte-derived dendritic cells (moDCs). An increase in the level moDCs occurs during viral respiratory infection or antigen presentation.
Scientists have pointed out a gap in research regarding the role of monocytes in providing protection against SARS-CoV-2 infection. A new study published in mBio addresses this gap by studying the role of monocytes in protecting individuals from SARS-CoV-2 by using a mouse-adapted SARS-CoV-2 (MA-SARS-CoV-2) strain and the human variant B.1.351. Additionally, the researchers have identified a CCR2-monocyte axis that is essential for controlling the virus and inhibiting inflammation within the respiratory tract during COVID-19 infection.
About the study
A previous study has identified a strong and reproducible connection between inflammatory cytokine levels and severe SARS-CoV-2 infection in humans. Similar to the result of the aforementioned study, the current study revealed that the SARS-CoV-2-infected mice possessed a proinflammatory cytokine profile. To this end, the lungs of infected mice contained chemoattractants for monocytes (Ccl2) and T-cells (Cxcl10), pyrogens (Il6 and Tnf), matrix metalloproteinases (Mmp14), interferon-stimulated genes (ISGs) (Irf7 and Isg15), and alarmins (S100a8).
Interestingly, the researchers also found that the expression of the inflammatory gene in the lung of MA-SARS-CoV-2 mice was dependent on the viral load. In this context, the researchers observed that cytokine transcripts studied by quantitative polymerase chain reaction (qPCR) were positively correlated with viral RNA. This finding agrees with a previous study using human subjects that described the relationship between SARS-CoV-2 viral load with IL-6 levels and an increased risk of death.
The researchers showed a substantial increase in the numbers of S100a8+ granulocytes in the lung parenchyma. Similarly, this finding is in line with studies associated with the analysis of the lung tissue or BAL fluids obtained from COVID-19 patients.
The present study reports an increased level of inflammatory cytokines and neutrophils in Ccr2−/− mice, which might be owing to elevated viral load in the lungs. This finding indicates that the MA-SARS-CoV-2 burden might be directly linked with cytokine expression and infiltration of neutrophils into the lungs.
Previous studies have shown that CCR2 expression is a determining factor of inflammatory Ly6C-high blood monocytes. This study reported that although CCR2 did not contribute to an increase in the numbers of circulating monocytes, it plays an important role in promoting the infiltration of activated monocytes into the lung parenchyma during COVID-19. The scientists also observed that inflammatory monocytes express a variety of chemokine receptors, like CXCR3.
Most importantly, this study highlighted the importance of CCR2 in promoting the recruitment and differentiation of monocytes into transitional macrophages and the rise in moDC during MA-SARS-CoV-2 infection. Despite the scientists of the current study focusing on the role of CCR2 only in monocyte-derived cells, it is also expressed in other types of cells such as natural killer cells and T-cells. In the future, more research on CCR2 signaling in other cell types and its role in both innate and adaptive immune responses is required.
The researchers revealed that as compared to other respiratory viruses like influenza, where CCR2 is associated with mortality and inflammation, in the context of COVID-19 infection, CCR2 limited viral burden and weight loss of infected mice. In the lung parenchyma, CCR2 promoted the infiltration of monocyte-derived cells.
Conclusion
The authors characterized a mouse model and highlighted that early CCR2-dependent infiltration of monocytes in the lungs is essential for controlling the viral load. This can also inhibit cytokine production during the early stages of MA-SARS-CoV-2 infection.
Therefore, taking into account the role of monocyte-derived cells in inhibiting COVID-19 in the lungs and priming adaptive immune responses, it could be effectively used in developing future therapies and vaccines.