The unprecedented coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has resulted in a massive global public health crisis. Many similarities have been observed between SARS-CoV-2, a beta coronavirus, and SARS-CoV, the causative pathogen of SARS.
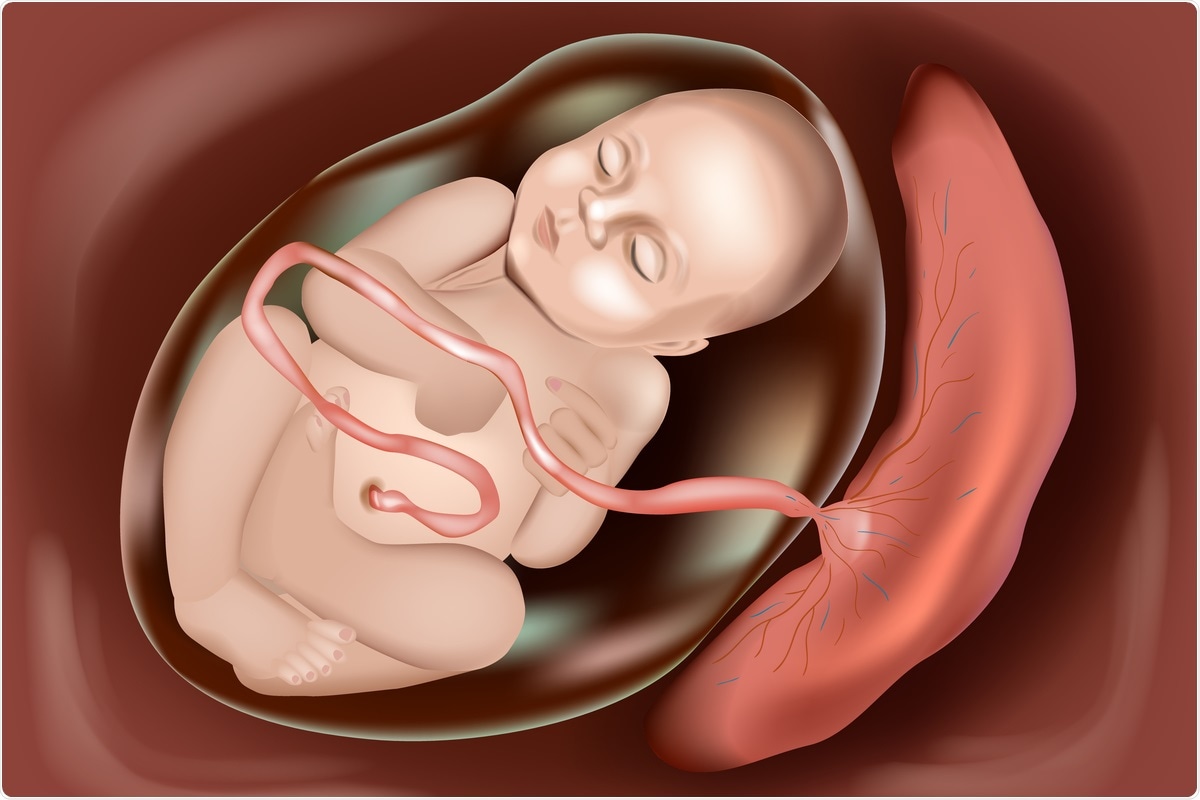 Study: SARS-CoV-2 can infect and propagate in human placenta explants. Image Credit: Sakurra / Shutterstock.com
Study: SARS-CoV-2 can infect and propagate in human placenta explants. Image Credit: Sakurra / Shutterstock.com
Background
Both SARS-CoV and SARS-CoV-2 mainly affect the upper and lower respiratory tract due to the abundance of the angiotensin-converting enzyme 2 (ACE2) receptor on the surface of the epithelial cells in the tract. Both viruses also use the endogenous plasma membrane serine protease TMPRSS2 for priming and activation. However, ACE2 and TMPRSS2 are also expressed in enterocytes, cardiomyocytes, endothelial cells, and placental trophoblasts, which indicates the wide cellular tropism of SARS-CoV-2.
Pregnant women are more prone to COVID-19 as compared to non-pregnant women of a similar age group. Various cohort studies have indicated that adverse events like stillbirth, pre-eclampsia, prematurity, and stillbirth were considerably increased in pregnant women with COVID-19.
Other reports also indicate that SARS-CoV-2 could severely affect fetal development due to placental pathological alterations. The precision-cut slices (PCSs) model was recently used by researchers to study the capacity of SARS-CoV-2 to infect and progress in the human placenta in the third trimester.
Assessment of the SARS-CoV-2 infection at the maternal-fetal interface
In a study recently published in the journal Cell Reports Medicine, the researchers report an ex vivo model, in which third-trimester placenta PCSs of 500 to 700 micrometer (mm) thickness were prepared and infected with SARS-CoV-2 or mock-treated and assessed after 24 to 120 hours of infection. The placenta PCS cultures were further characterized to visualize syncytiotrophoblasts and cytotrophoblasts by using B-cell lymphoma 2 (BCL-2) and trophoblast cell-surface antigen 2 (TROP-2), respectively. Additionally, well-differentiated primary human nasal epithelial cells (WD-NECs) cultured at the air-liquid interface (ALI) were used as a positive control.
Interestingly, SARS-CoV-2 was fully replicated in placenta PCSs with the release of infectious viral particles. The vulnerability of the human placenta to SARS-CoV-2 replication could be attributed to the extent of the high levels of ACE2 expression.
SARS-CoV-2 proteins were also identified in cytotrophoblasts, villous stroma, syncytiotrophoblast, and probably Hofbauer cells, thus confirming the broad cell tropism of SARS-CoV-2. The researchers observed no cytotoxicity and pro-inflammatory cytokine response in SARS-CoV-2 infected placenta PCSs; however, higher levels of interferon type III transcripts were noted.
“Remarkably, we found a significant association between ACE2 levels and placenta permissiveness to SARS-CoV-2 infection.”
Conclusions
The current study analyzed the interaction of SARS-CoV-2 at the human maternal-fetal interface by using an advanced ex vivo model. The findings elucidated the vulnerability of the human placenta to SARS-CoV-2 due to high ACE2 expression levels. This model could be used as a platform to screen anti-SARS-CoV-2 drugs that can target the placenta.
The observations showed the capacity of SARS-CoV-2 to infect and replicate in the human placenta in the third trimester. They highlight the need for further investigations into the measures that can be used to protect women from the adverse events associated with COVID-19 during pregnancy.
“We demonstrated with independent methods the susceptibility of the human 161 placenta towards SARS-CoV-2 infection with the release of replication-competent virions.”
Limitations
Although this experimental approach allows the study of the interaction between SARS-CoV-2 and the human placenta, the model is not appropriate for assessing the placental barrier or the influence of immune components on long-term outcomes. Since the work used a third-trimester placenta, the findings discussed here do not reveal much about SARS-CoV-2 replication during early pregnancy.
Additionally, the study could not explain the mechanism by which SARS-CoV-2 reaches the placenta. Lastly, although the virus was found in the serum or plasma of COVID-19 patients, there is no data regarding the presence of infectious viral particles in peripheral blood.
Journal reference:
- Fahmi, A., Brügger, M., Démoulins, T., et al. (2021). SARS-CoV-2 can infect and propagate in human placenta explants. Cell Reports Medicine. doi:10.1016/ j.xcrm.2021.100456.