The ongoing coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), has affected healthy pregnancies. Researchers have found that pregnant women get infected with this virus and experience mild, asymptomatic, or critical illness. According to one study, acute SARS-CoV-2 infection and mortality in pregnant women were higher than in non-pregnant women.
Besides the tendency of severe infection in pregnant women, an increased risk for stillbirth, preterm birth, preeclampsia, and low birth weight has been associated with expectant mothers with SARS-CoV-2 infection. However, previous studies have indicated that vertical transmission of SARS-CoV-2 from mother to fetus during pregnancy is a rare occurrence.
Researchers have also estimated positive neonatal nasopharyngeal via PCR test, and the rates were found to be ranging between 0.5 and 2.5%. The SARS-CoV-2 virus was also detected in the placental tissues, i.e., placental trophoblast cells in vitro. The link between the rarity of fetal transmission and the presence of the virus in the placental tissues indicated the presence of vital factors that prevented the transplacental passage of SARS-CoV-2.
Scientists highlighted the significance of intrauterine immune responses that are primarily governed by maternal leukocytes in the decidual tissues adjacent to the villous placenta. Some immune cells, such as decidual T cells, natural killer cells, and macrophages, respond to viral infection at the maternal-fetal interface. They provide protection either through cellular (direct) or cytokine-mediated pathogen-specific responses (indirect).
Prior studies revealed sexually dimorphic modifications in interferon response genes as well as inflammatory responses in the villous placental tissue of pregnant women infected by SARS-CoV-2 in the third trimester of pregnancy. However, a complete understanding of the leukocyte and cytokine profiles related to the decidual-specific immune response in SARS-CoV-2 infected pregnant women is required, especially before the third trimester.
A New Study
Scientists have hypothesized that the number of immune cells and the amount of cytokines produced in response to SARS-CoV-2 infection in pregnant women change in accordance with the timing of maternal infection in pregnancy. This study is available on the bioRxiv* preprint server.
In the current study, researchers evaluated the decidual leukocytes and cytokine profiles using decidual tissues from women with symptomatic SARS-CoV-2 infections in their second or third trimesters of pregnancy.
These results were compared with the control group, which helped characterize the trajectory of the decidual immune responses against SARS-CoV-2 infection at the maternal-fetal interface.
Main Findings
The current study showed an association between SARS-CoV-2 infection during pregnancy and an enhancement in a specific type of immune cell found to be dependent on gestational timing of infection.
Researchers also successfully profiled cytokine levels and correlated with macrophage abundance at third-trimester SARS-CoV-2 infections. Additionally, an overall inclination of downregulation in the pro and anti-inflammatory cytokine production was reported in pregnancies with second-trimester maternal COVID-19 disease.
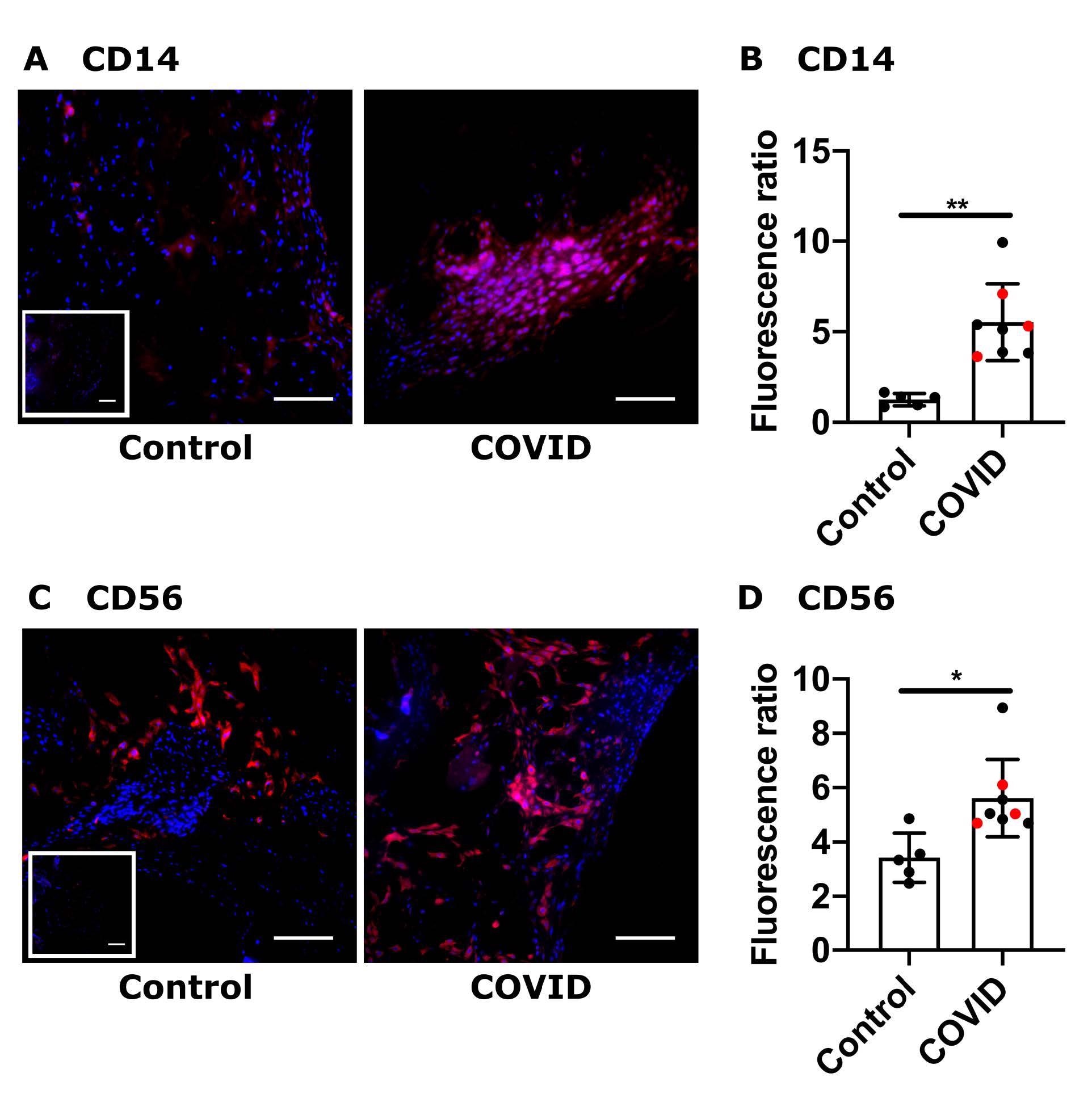 Placental maternal immune cell infiltrates from retrospective COVID-19 cohort. (A, C) Representative images (200x) of decidual areas stained for (A) CD14 (red) or (C) CD56 (red) immunofluorescence. (B, D) Graphical analysis of comparative fluorescence quantitation of (B) CD14 and (D) CD56. Red circles indicate dyads with an infant who tested positive for SARS-CoV-2 by nasal PCR swab at 24 or 48 hours of life. SARS-CoV-2 positive (COVID, n = 8) or negative (control, n = 5). * p <0.05; ** p <0.01. Scale bar: 50μm; insets: secondary-only controls.
Placental maternal immune cell infiltrates from retrospective COVID-19 cohort. (A, C) Representative images (200x) of decidual areas stained for (A) CD14 (red) or (C) CD56 (red) immunofluorescence. (B, D) Graphical analysis of comparative fluorescence quantitation of (B) CD14 and (D) CD56. Red circles indicate dyads with an infant who tested positive for SARS-CoV-2 by nasal PCR swab at 24 or 48 hours of life. SARS-CoV-2 positive (COVID, n = 8) or negative (control, n = 5). * p <0.05; ** p <0.01. Scale bar: 50μm; insets: secondary-only controls.
Researchers reported an association between COVID-19 in the third trimester and increased macrophage, natural killer cell, and T cell populations. However, in the second trimester, increased T cell populations were observed. This study included a second-trimester infection group, along with long-term immune consequences at the maternal-fetal interface. These aspects are critical, as very few studies are available in this regard.
The authors indicated an increase in the T cell infiltration in both 10 weeks and 21 weeks following infection. In the future, phenotypic characterization of the T cells must be conducted to understand their specific functions.
Downregulation of pro-inflammatory cytokines in the placenta following second-trimester COVID-19 was reported which might be caused by the tissues being in the resolution phase post-infection.
Although in the cytokine analysis, the authors expected that pro-inflammatory cytokines would be enhanced in the decidual tissues from women with third-trimester COVID-19, it was not the case. Instead, no important differences, with the exception of IL-8 downregulation, were observed. This result is in line with a previous study that reported no significant changes in pro-inflammatory cytokines levels associated with COVID-19 in pregnancy, at the placental level for TNF-a, IL-1b, or IL-6.
Conclusion
The authors highlighted some of the limitations of the current study. One of the study's shortcomings is related to the timing of sample collection, i.e., it is plausible that the participants of the study were severely infected during the first wave of COVID-19, limiting the generalizability of these results.
Another limitation includes a small sample size that was collected from a single clinical site. Scientists recommended that more studies conducting a complete evaluation of immune profile in pregnancies affected by maternal COVID-19 are required.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources