Due to the rapid human-to-human transmission and predominance of asymptomatic carriers, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) remains an international public health concern, despite the implementation of many interventions to slow its spread.
Many countries established physical separation protocols and/or lockdown limitations at the beginning of the coronavirus disease 2019 (COVID-19) pandemic. Simultaneously, diagnostic assays were rapidly developed fast and given emergency use authorization (EUA) by the United States Food and Drug Administration (FDA) to identify people with active SARS-CoV-2 infections.
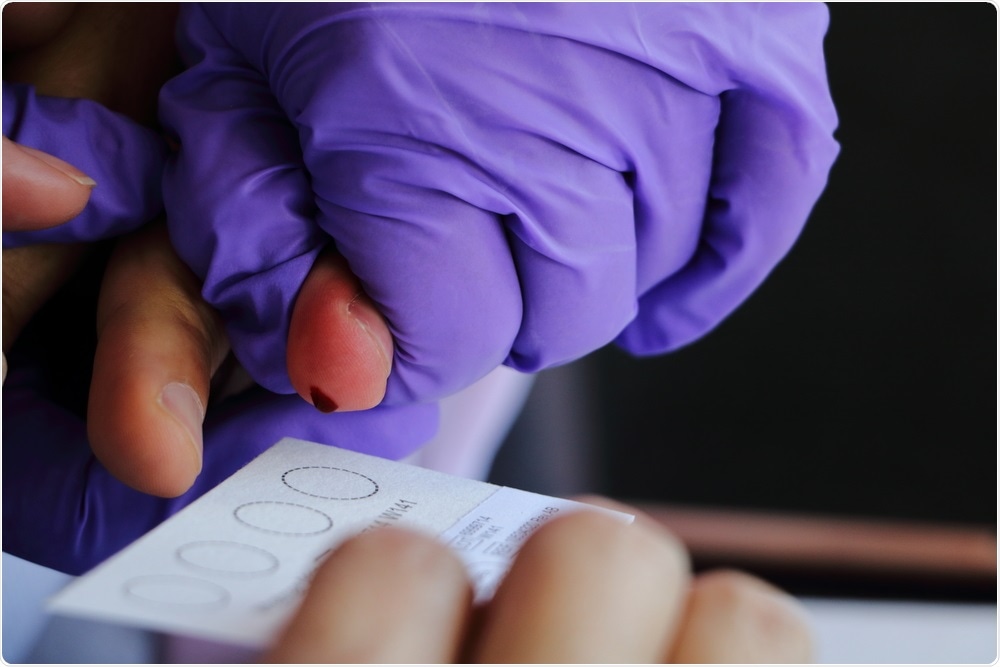 Study: Monitoring of SARS-CoV-2 Antibodies Using Dried Blood Spot for At-Home Collection. Image Credit: worawot300 / Shutterstock.com
Study: Monitoring of SARS-CoV-2 Antibodies Using Dried Blood Spot for At-Home Collection. Image Credit: worawot300 / Shutterstock.com

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Background
Although social distancing and diagnostic testing remain critical to reducing the spread of SARS-CoV-2, the introduction of COVID-19 vaccinations offers a more reliable approach to restrict viral transmission. Vaccines work by inducing the body's natural immune response, which results in the production of antibodies that can neutralize the virus, subsequently reducing the severity of infections and transmission of the virus.
Many laboratories and researchers have examined the use of dried blood spot (DBS) collection for both qualitative and quantitative detection of SARS-CoV-2 antibodies since the beginning of the outbreak. When comparing DBS results to plasma or serum in proof-of-concept trials, these tests showed good sensitivity and specificity. However, more research, including studies based on regulatory advice, is needed before DBS samples can be used for at-home self-collection.
The results presented in the current study, which is published on the preprint server medRxiv*, constitute a more thorough examination of this assay as compared to previous studies, with a streamlined extraction technique, a lower reporting limit for DBS samples, and evidence of sample self-clustering.
About the study
CLSI EP17-A2 advice was used to assess the detection capabilities of the assay with DBS extracts. Over the course of four days, two different reagent lots were utilized to produce 96 blank assays on six fabricated blood samples.
The z-score for each of these outcomes, in relation to the remaining results, was larger than 4.7 for both reagent lots; thus, they were excluded from the data analysis. The limit of blank (LOB) for DBS extracts was calculated using the mean and standard deviation of the remaining blank results, as well as a normal distribution multiplier.
The limit of quantitation (LOQ) of DBS extracts was determined using 14 fabricated blood samples spanning an appropriate concentration range between 0.0528 and 0.648 U/mL. Over a five-day period, these samples were extracted and measured in triplicate using two different reagent lots on a single instrument. The target total variance (CV) and bias for this study were set to 25.0%, which is based on FDA guidance for ligand binding assays at the lower limit of quantitation.
Following data collection, the imprecision profiles were analyzed in EP Evaluator® using the Limit of Quantitation module. These results showed that the first reagent lot had a LOQ of 0.0873 U/mL, while the second reagent lot had a LOQ of 0.0736 U/mL.
Furthermore, for all levels greater than the DBS limit of detection (LOD), acceptable biases of less than 25.0% were observed. Because both imprecision and bias results indicate a LOQ less than the observed LOD, the LOQ for DBS extracts is effectively equal to the LOD of 0.180 U/mL.
In eight donors, self-collected DBS samples were used in conjunction with serial measurement of SARS-CoV-2 antibody levels after immunization. Donors collected DBS samples on a regular basis from before immunization to 19 weeks after the first vaccination.
The Pfizer-BioNTech COVID-19 vaccination was administered to all donors, with the second dose administered exactly three weeks after the first. For samples collected within the first nine days after the first immunization, all donors reported negative DBS findings. Between days 10 and 16, each donor's antibody levels rose beyond the DBS limit of 0.185 U/mL.
Following the second vaccination dose, antibody levels increased rapidly, with several donors exceeding the DBS reporting limit of 250 U/mL, which is calculated to be 3,570 U/mL in serum. Donor seven had significantly lower antibody levels, which were most likely caused by the immunosuppressive medication the donor reported taking for a chronic condition.
Implications
The comprehensive results presented in this study show that using DBS samples to measure SARS-CoV-2 antibodies is a reliable method. Although DBS samples are diluted during the extraction procedure, this method has benefits. Sample-to-sample matrix effects were decreased, and a lower reporting LOQ of 0.180 U/mL for DBS samples was obtained when Roche's Universal Diluent was used as the extraction buffer.
Furthermore, the dilution of the sample allowed for a broader relative measurement range, as a DBS sample with a maximum concentration of 250 U/mL would be greater than 3,500 U/L in blood. These findings, together with a strong correlation to venous serum data, allowed the assay to be utilized to demonstrate antibody tracking over time using DBS self-collection at home.
When antibody levels inferring protective immunity are better understood, DBS samples may become an essential tool for frequent antibody monitoring and scheduling of vaccination boosters.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources