The World Health Organization (WHO) declared a pandemic on March 11, 2020, due to the rapid spread of the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). As a result, peripartum women were subject to unique health concerns and interruptions in perinatal care.
Although a rise in maternal morbidity has been documented among both women with and without COVID-19, little is known about the outcomes of childbirth among Black and Latinx individuals during the coronavirus pandemic.
In new research, scientists studied individuals who gave birth during COVID-19. Using propensity score matching (PSM), they matched those identified as either Black or Latinx with those identified as non-Hispanic white on sociodemographic. This recent study published as a preprint on the medRxiv* server attempts to assess the impact of the COVID-19 pandemic on childbirth-related health outcomes in individuals belonging to Black or Latinx minority groups.
Disparities in obstetric outcomes are well documented during the pre-pandemic period, and Black and Latinx individuals have been found to be at higher risk of maternal mortality and developing life-threatening complications.
Additionally, there is also a higher occurrence of maternal mental health issues such as peripartum depression in this population.
 Study: Racial and ethnic disparities in maternal mental health during COVID-19. Image Credit: Zhuravlev Andrey / Shutterstock
Study: Racial and ethnic disparities in maternal mental health during COVID-19. Image Credit: Zhuravlev Andrey / Shutterstock

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
How was the study conducted?
The present study was a part of the maternal wellness project that commenced on April 2, 2020. It was conducted on 236 women belonging to the minority groups Black/African American or Hispanic/Latinx and 236 women belonging to the non-Hispanic group.
The women selected for the study had given birth in the last six months, and they were asked to complete an anonymous survey on childbirth and mental health.
The average age of the participants was 31 years old, and the participants were on an average 2 months postpartum. Of the participants, 83.7% resided in the US, 54.2% belonged to middle-class income, 78.2% were married, 65.1% had a college degree, 95.6% delivered a healthy baby at term and, 53.2% were primiparas (bearing the first offspring).
Propensity score matching was employed to match sociodemographic factors in the Black or Latinx group with the non-Hispanic white group and subsequently, the groups were compared to assess the impact of COVID-19 on childbirth-related health outcomes.
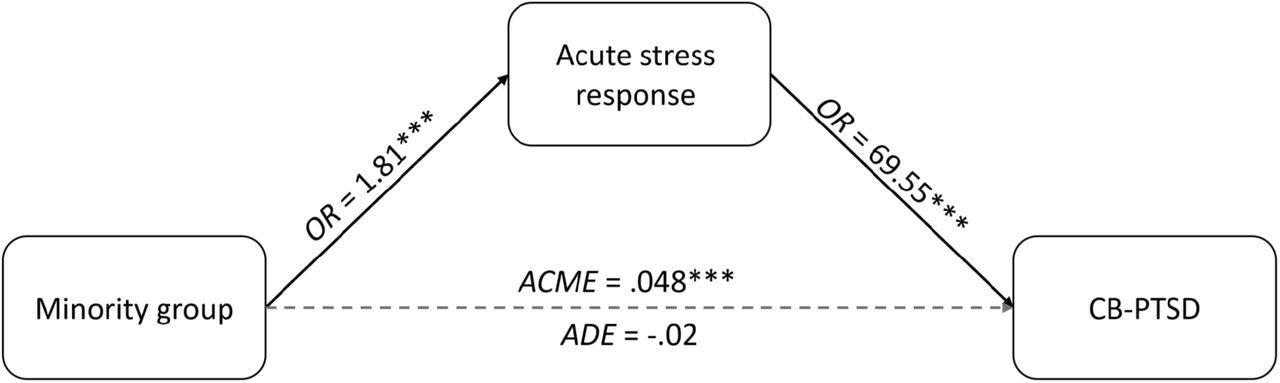 Acute childbirth-related traumatic stress response significantly mediates the effect of minority group on the likelihood of developing childbirth-related posttraumatic stress disorder (CB-PTSD). OR = odds ratio, ACME = average causal mediated effect, ADE = average direct effect.
Acute childbirth-related traumatic stress response significantly mediates the effect of minority group on the likelihood of developing childbirth-related posttraumatic stress disorder (CB-PTSD). OR = odds ratio, ACME = average causal mediated effect, ADE = average direct effect.
What are the findings from the study?
When compared to the Non-Hispanic white individuals, the minority groups had a higher risk of developing postpartum depression. Notably, there was no difference in the occurrences of history of depression between both groups. However, a significant difference in the occurrence of postpartum depression existed between the groups even after controlling for factors such as the history of mental health, abuse, and complications in recent childbirth.
The minority group had a higher risk of clinically significant traumatic stress response to childbirth and higher rates of unplanned caesareans.
Further, lower incidences of immediate skin-to-skin contact, rooming-in and breastfeeding were also observed in the minority group.
In the minority group occurrence of acute traumatic stress to childbirth was significantly associated with childbirth-related post-traumatic stress disorder (CB-PTSD).
Implications of the present study
In the study, Black and Latinx women who gave birth during the COVID-19 pandemic had a higher rate of maternal psychiatric morbidity than their white counterparts. This rate remained high even after adjusting for confounding factors such as pre-morbid mental health, histories of abuse, and complications during recent childbirth.
The study also identified an increased risk of unplanned cesarean deliveries in minority women, which may result in higher rates of morbidity during childbirth. Further, the mothers may not be able to engage in postpartum bonding behaviors such as skin-to-skin contact and breastfeeding, which contribute to the development of a healthy child. Maternal and infant health may differ between ethnic and racial groups as a result of these factors.
The study found that individuals from the Black and Latinx group have a higher risk of experiencing trauma during childbirth. One-third of the study subjects in the Black and Latinx group had reported experiencing clinically significant acute stress as a response to childbirth. The risk of occurrence was three times higher in the minority group than the non-Hispanic white individuals. In addition, individuals in the minority group had two times more risk of developing postpartum depression that requires clinical monitoring.
Adverse maternal outcomes may result due to structural inequities and racism. Social and economic inequalities can result in disparities in health care access. However, sociodemographic factors have not prevented the emergence of gaps in pregnancy-related morbidities. This was observed in the present study where gaps existed in maternal mental health and maternal bonding behaviors despite adjusting for factors such as income, education, geographic location, and abuse history. History of mental health or complications during recent childbirth did not also explain the observed gaps. This indicates that exposure to stressors that may negatively impact adaptive coping behavior may not be responsible for the observed adverse maternal outcomes. Various parameters in the health care system may be promoting the impact of racism on birth outcomes.
Conclusion
The findings of this study indicate that Black and Latinx women who gave birth during the COVID-19 pandemic were more likely to experience mental health morbidity after childbirth. In order to enhance the mental health outcomes of individuals who belong to minority groups after childbirth, measures should be taken to support postpartum adjustment. Clinical practice and public policy changes must be implemented that address the gaps that can lead to adverse maternal health outcomes such as childbirth-associated mental health morbidities.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.