Several reports have shown that the effectiveness of the Pfizer BNT162b2 vaccine against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) declined after the emergence of the SARS-CoV-2 Delta variant (B.1.617.2). This led to a surge in coronavirus disease (COVID-19) cases in people who received a two-dose regimen of the Pfizer vaccine as soon as the vaccine became available.
The Israeli Ministry of Health approved the use of a booster dose of the Pfizer vaccine on July 30, 2021, to mitigate the resurgence in COVID-19 cases. However, evidence on the effectiveness of booster doses in decreasing COVID-19 mortality is insufficient.
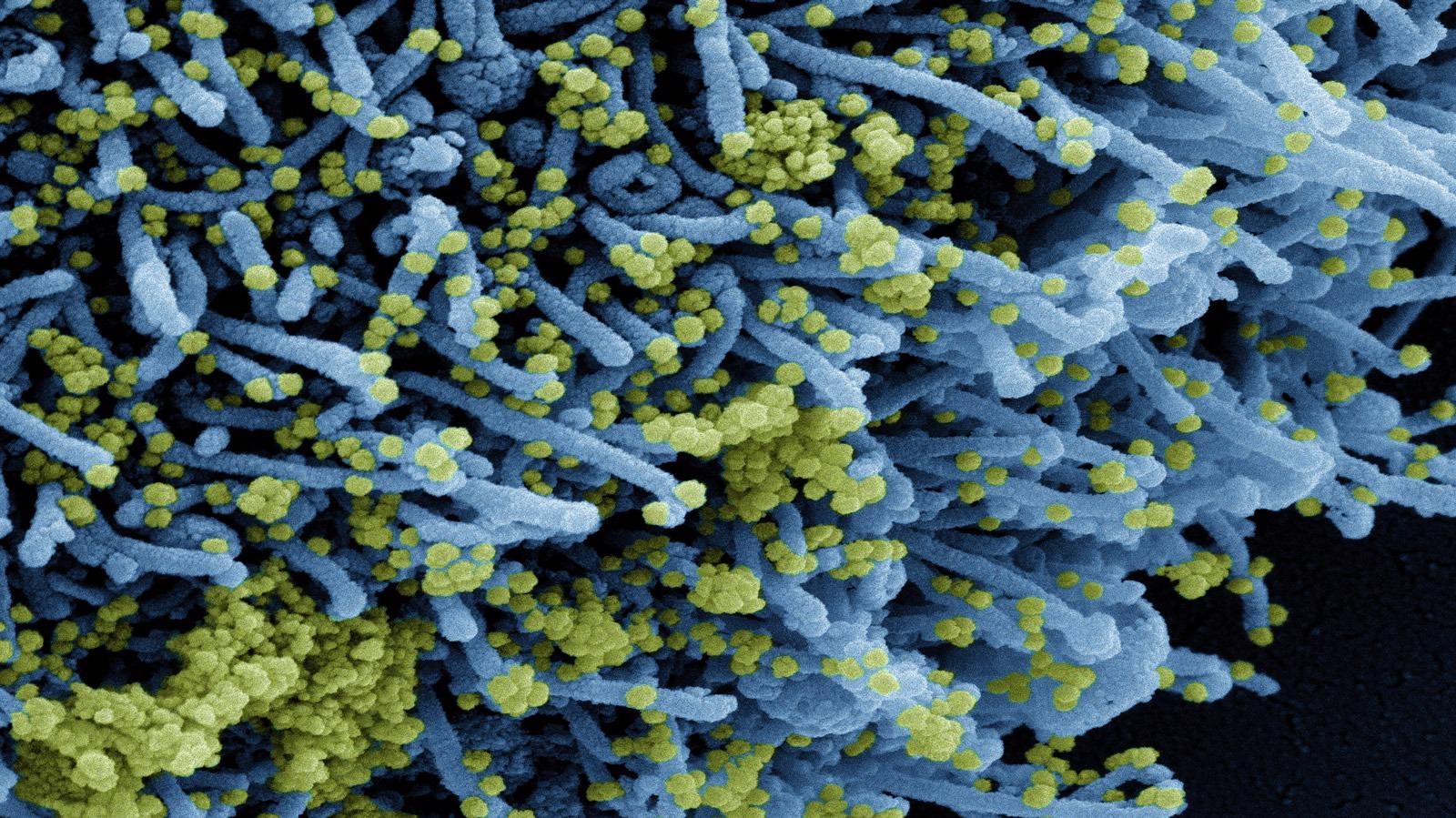 Study: BNT162b2 Vaccine Booster and Mortality Due to Covid-19. Image Credit: NIAID
Study: BNT162b2 Vaccine Booster and Mortality Due to Covid-19. Image Credit: NIAID
About the study
A recent observational study conducted from August 6, 2021, to September 29, 2021, in Israel evaluates the efficacy of a Pfizer vaccine booster dose in reducing the mortality rate of COVID-19. The study participants were members of the Clalit Health Services (CHS), were 50 years or older at the beginning of the study, and had received a two-dose regimen of the Pfizer vaccine at least five months before the study. The research is published in the New England Journal of Medicine.
The exclusion criteria for study subjects included those without proper data regarding the gender or date of birth, prior SARS-CoV-2 infection, those who received a booster dose before the start of the study, and those who received a booster dose and were positive for COVID-19 within three days before the effective-booster date, which is otherwise a week after the booster dose was administered.
The study subjects were divided into two groups based on those who received a booster dose (booster group) and those who did not receive the booster dose (non-booster group). The COVID-19 mortality rate among them was compared.
Between the dates of booster and effective-booster dose, there was a lag of seven days. The validation of this lag period ensured that the effectiveness of the booster dose was maintained throughout the study.
Variables that can be used as inputs for univariate and multivariate regression analysis were obtained by using a chi-square test and Kaplan-Meier analysis. The association of COVID-19 mortality and the efficacy of booster dose was estimated using a Cox proportional-hazard regression model with time-dependent covariates after adjusting factors like the sociodemographic and coexisting conditions.
Study findings
During the study period, out of the 843,208 subjects who met the inclusion criteria, 758,118 participants, which amounted to nearly 90%, received the booster dose. The majority of the study participants were 65 years or older and had comorbidities such as hypertension, obesity, and diabetes.
COVID-19-associated death occurred in 137 subjects of the non-booster group compared to only 65 subjects in the booster group. A total of 2,888 individuals in the booster group had confirmed COVID-19, while 11,108 non-booster group participants were positive for COVID-19.
Age, male gender, chronic renal failure, lung cancer, and a prior incidence of cerebrovascular events were risk factors in COVID-19-related mortality according to the Cox regression model. The history of smoking, socioeconomic status, and comorbidities like chronic obstructive pulmonary disease, diabetes, obesity, chronic heart failure, and ischemic heart disease were not significantly associated with COVID-19 related death.
The findings of the current study demonstrate that those who received a Pfizer vaccine booster dose at least five months after the second vaccine dose had a 90% lower chance of COVID-19-related mortality compared to the non-booster population.
Conclusions
According to this study, there was a 90% reduction in COVID-19-related death in those who received the Pfizer vaccine booster dose after five months of the second dose. The study results provide crucial data on the significant lifesaving potential of booster doses, which could help decision-making on booster vaccine policy.
A preliminary study previously conducted by the Israeli Ministry of Health evaluating the efficiency of Pfizer vaccine boosters in reducing COVID-19-associated death showed a 93% lower death rate as compared with the 90% lower death rate in the present study. The variation in these results may be due to differences in study designs, lag time, database, and monitoring period.
The present study had some limitations such as the short duration of 54 days, the evaluation of only the Pfizer vaccine booster efficacy among several other COVID-19 vaccines with different waning patterns, and the lack of information regarding the adverse effects of the vaccine. Similarly, there may be bias in the socioeconomic and clinical variables, as well as the estimation of survival rate.
The authors suggested the evaluation of the safety profile of booster dose administration in future studies and believe that more studies with long-term monitoring periods are necessary to assess the effectiveness and safety of the booster doses.
Journal reference:
- Arbel, R., Hammerman, A., Sergienko, R., et al. (2021). BNT162b2 Vaccine Booster and Mortality Due to Covid-19. The New England Journal of Medicine. doi:10.1056/NEJMoa2115624.