During the earlier phases of the ongoing coronavirus disease (COVID-19) pandemic, several remote home-based monitoring programs were set up in England for detecting early signs of deterioration in people with COVID-19 using pulse oximetry. Ultimately, these programs aimed to safely manage patients outside of the hospital, as well as provide reassurance and prompt escalation where necessary.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
To this end, the National Health Service (NHS) launched community-based home monitoring services that were referred to as ‘COVID Oximetry @ home’ (CO@h) during the second COVID wave in 2020. CO@h focused on managing COVID-19 patients with mild-to-moderate symptoms diagnosed in the community and was focused on self-escalation and more appropriate admissions.
Thereafter in January 2021, a national launch of post-hospital discharge ‘COVID Virtual Ward’ (CVW) models was introduced. These were intended to support the early discharge of hospitalized and severely ill patients, as well as prevent unnecessary readmissions.
About the study
A new study posted to the medRxiv* preprint server discusses the impact of the implementation of CO@h models in other settings and assesses the impact of post-hospital discharge CVW models.
The following questions were to be addressed:
- What was the impact of CVW on the length of stay of COVID-19 hospitalizations?
- What was the impact of CVW on rates of subsequent readmission for COVID-19?
- Were there any associations between patient characteristics and hospital outcomes?
Here, information was extracted on all individuals who recovered in 123 English hospital trusts where there had been a confirmed or suspected COVID-19 ICD-10 diagnosis code from Hospital Episode Statistics Admitted Patient Care (HES APC) data.
All patients discharged from August 17, 2020, to February 28, 2021, were included. Importantly, this period marked the entire second COVID-19 wave in England.
Overall, 139,619 patients with a primary diagnosis of COVID-19 were discharged during the study period. As some patients were hospitalized multiple times, these discharges attributed to 129,461 individuals. The present analysis included 98.2% of all patients with a primary COVID-19 diagnosis discharged from various institutions in England.
Study findings
The age range of patients who were discharged where a CVW was available was 50-64 years. Discharges of patients where a CVW was available were more likely to be occurring due to the higher levels of beds occupied by COVID-19 patients.
The mean length of stay (LOS) for patients discharged where a CVW was available was 10.1 days as compared to 8.9 days for patients where a CVW was not available. After adjusting for all covariates, the incidence rate ratio (IRR) of 1.05 was estimated for discharges where a CVW was available as compared to those where a CVW was not available. Thus, the LOS was 5% longer for relevant COVID-19 inpatients where a CVW had been available.
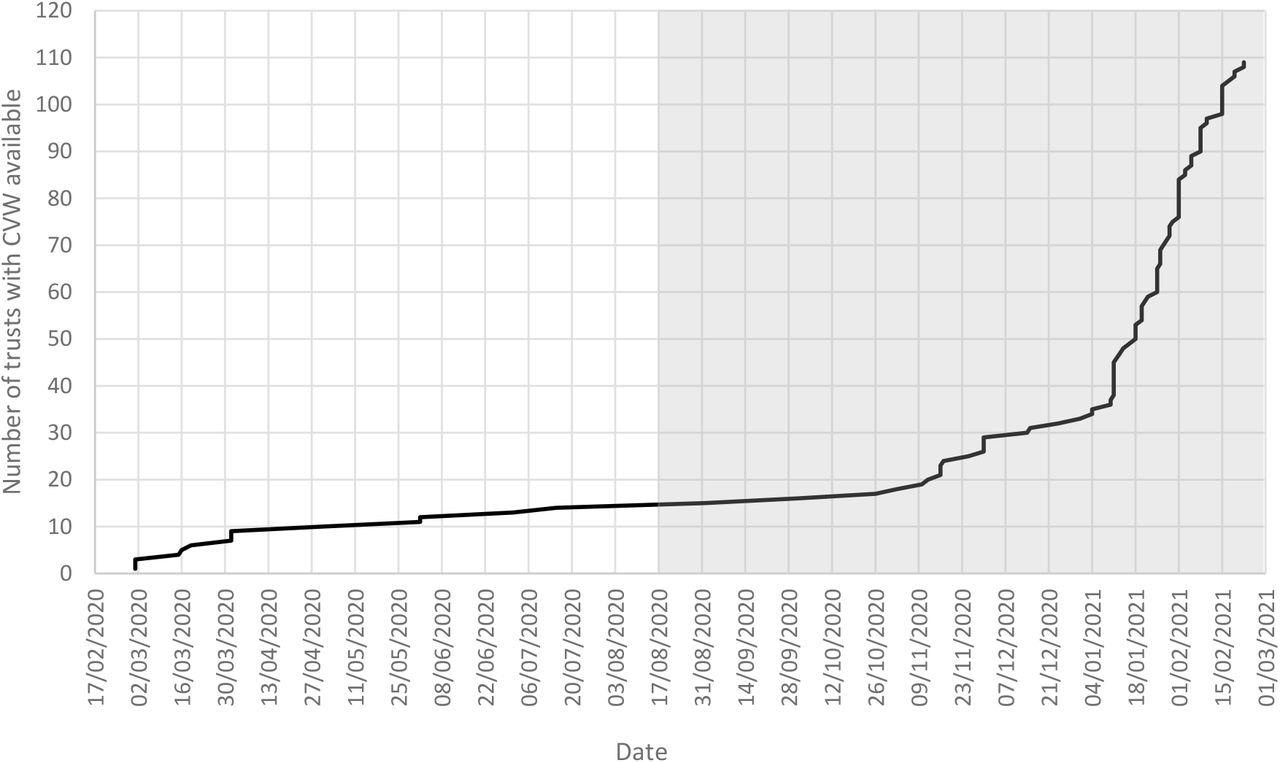
Cumulative start dates of CVW services in England’s non-specialist acute hospital trusts (n = 123 trusts). 14 trusts had no CVW by 22 February 2021. The grey box represents the main period of this analysis.
Additionally, people living in the most affluent population quintiles tended to have slightly shorter LOS than those in the most deprived circles. Moreover, the first inpatient stay due to a primary COVID-19 diagnosis was longer than the subsequent stays. Meanwhile, the LOS showed a decreasing trend as the proportion of acute beds occupied by COVID-19 patients increased.
Among the patients discharged from trusts with a CVW available, 3.0% had readmissions with COVID-19 within 28 days. Comparatively, the rate was 13·2% among patients discharged from trusts where no CVW was available. However, after adjusting for all variables, the difference was found to be insignificant.
The relative odds of readmission and LOS increased proportionately with the patients’ increasing age. Females had a significantly lower predilection to readmission than males, whereas Black patients had a lower predilection for readmission as compared to Whites. There were no apparent differences in readmissions among patients residing in less deprived areas as compared to the most deprived areas.
Taken together, the study findings did not provide any evidence of early discharges or reduced rates of hospital readmissions associated with the COVID Virtual Wards in England. The results are speculated to project the true impact of the service. Nevertheless, the effects of a lack of data on which patients had been enrolled, the COVID-19 in-hospital treatments, and clinical observations cannot be overlooked.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Georghiou, T., Sherlaw-Johnson, C., Massou, E., et al. (2022). The impact of post-hospital remote monitoring of COVID-19 patients using pulse oximetry: a national observational study using hospital activity data. medRxiv. doi:10.1101/2022.01.11.22269068. https://www.medrxiv.org/content/10.1101/2022.01.11.22269068v1.
- Peer reviewed and published scientific report.
Georghiou, Theo, Chris Sherlaw-Johnson, Efthalia Massou, Stephen Morris, Nadia E. Crellin, Lauren Herlitz, Manbinder S Sidhu, et al. 2022. “The Impact of Post-Hospital Remote Monitoring of COVID-19 Patients Using Pulse Oximetry: A National Observational Study Using Hospital Activity Data.” EClinicalMedicine 48 (June): 101441. https://doi.org/10.1016/j.eclinm.2022.101441. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(22)00171-7/fulltext.