Although SARS-CoV-2 is mainly transmitted via respiratory droplets, potential aerosol transmission has been reported under some conditions. However, comprehensive information regarding SARS-CoV-2 viral load in exhaled breath samples, the size and concentration of the exhaled droplets, and the relation between the aerosol samples and viral load in upper airway diagnostic samples are limited.

Study: Severe acute respiratory syndrome coronavirus 2 can be detected in exhaled aerosol sampled during a few minutes of breathing or coughing. Image Credit: Gustavo Tabosa / Shutterstock
About the study
In the current study, the researchers counted and gathered endogenous particles in exhaled breath in COVID-19 patients during 10 airway opening breaths, 20 normal breaths, and three coughs. Breath samples obtained from the subjects were analyzed using reverse transcription real-time polymerase chain reaction (RT-PCR).
The researchers used two impaction-based methods: 1) the particles in exhaled air (PExA) method and 2) the Breath Explor (BE) aerosol-collection device. They compared the SARS-CoV-2 viral load in aerosol exhaled during various types of breathing and coughing and analyzed how SARS-CoV-2 infection influences the size and number of exhaled particles less than 5 μm.
This study comprised two substudies - the first during September–October 2020 and the second from April to May 2021. While the first substudy included mild COVID-19 cases, the second one included SARS-CoV-2-positive health care workers at the Sahlgrenska University Hospital, Gothenburg, Sweden. The diagnosis was confirmed using RT-PCR analysis of a combined oro/nasopharyngeal swab sample in the first substudy, while a positive rapid COVID-19 antigen test in nasopharyngeal swab samples was used to confirm the diagnosis in the second substudy.
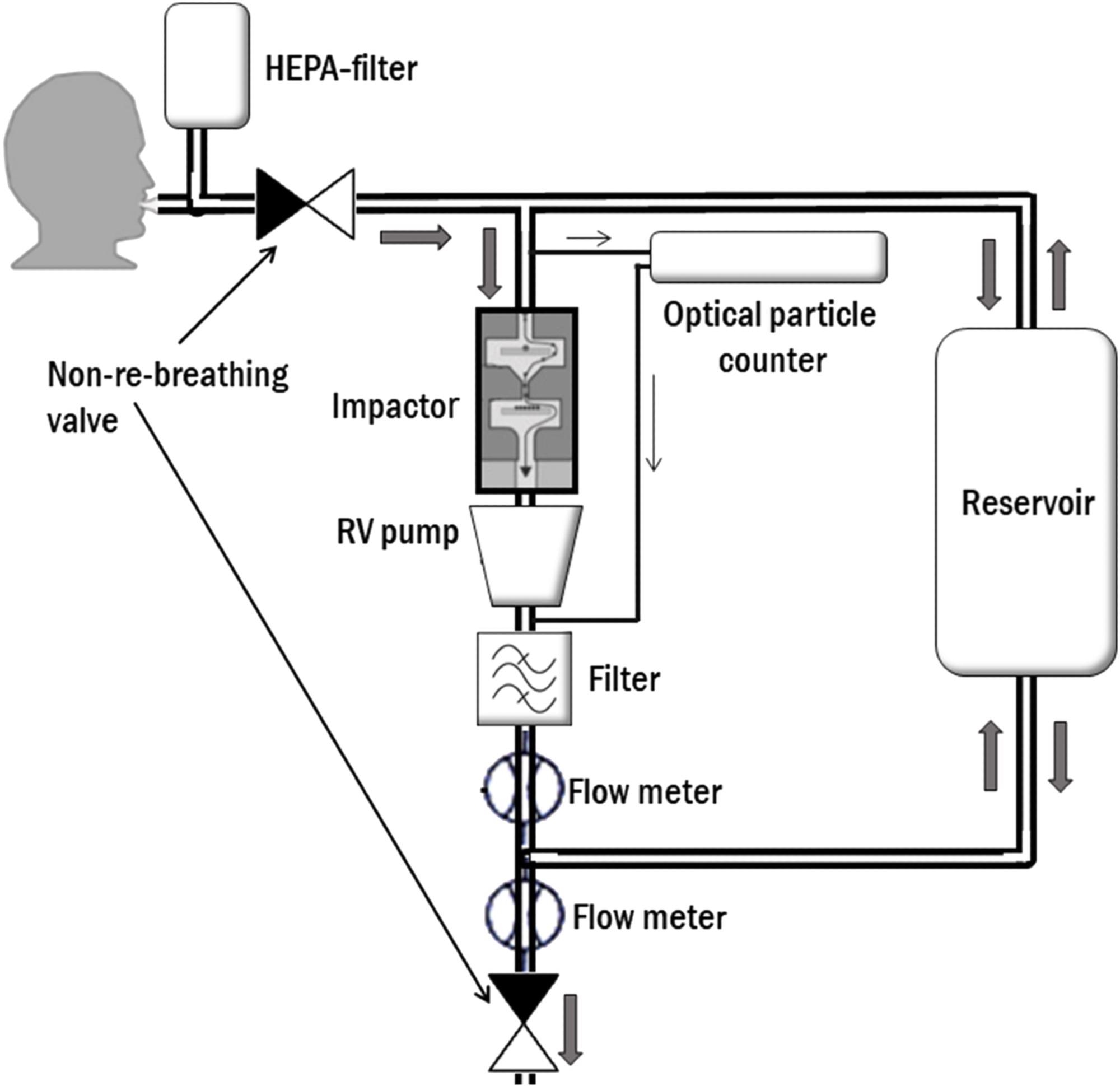 Schematic illustration of the particles in exhaled air (PExA) instrument set-up at collection. Subject breaths through a mouthpiece, connected to a two-way, non-re-breathing valve, where inhalation goes through a high-efficiency particle arresting (HEPA) filter, and exhalation go into the instrument. An optical particle counter samples a fraction of the exhaled air with a constant flow of 20 ml/s. The two-stage inertial impactor collects particles according to size by the control of a rotary vane (RV) pump with a constant flow of 230 ml/s. A reservoir handles exhalations that exceed the flow rate through the impactor
Schematic illustration of the particles in exhaled air (PExA) instrument set-up at collection. Subject breaths through a mouthpiece, connected to a two-way, non-re-breathing valve, where inhalation goes through a high-efficiency particle arresting (HEPA) filter, and exhalation go into the instrument. An optical particle counter samples a fraction of the exhaled air with a constant flow of 20 ml/s. The two-stage inertial impactor collects particles according to size by the control of a rotary vane (RV) pump with a constant flow of 230 ml/s. A reservoir handles exhalations that exceed the flow rate through the impactor
Results
Combined PExA and BE results showed that the SARS-CoV-2 RNA was detected in aerosols of 10 (40%) out of the 25 subjects, which indicates that SARS-CoV-2 RNA was not detected in exhaled particles from all subjects with early COVID-19 disease. The presence of viral RNA in aerosol was found in eight cough samples, three airway opening breaths, and four normal breaths, without any overlap between the methods.
There was no association between the number of exhaled particles less than 5 μm and the viral load in aerosols. Study participants with COVID-19 exhaled fewer particles than healthy controls during airway opening breaths and normal breathing (P < 0.05), although this was not true during cough.
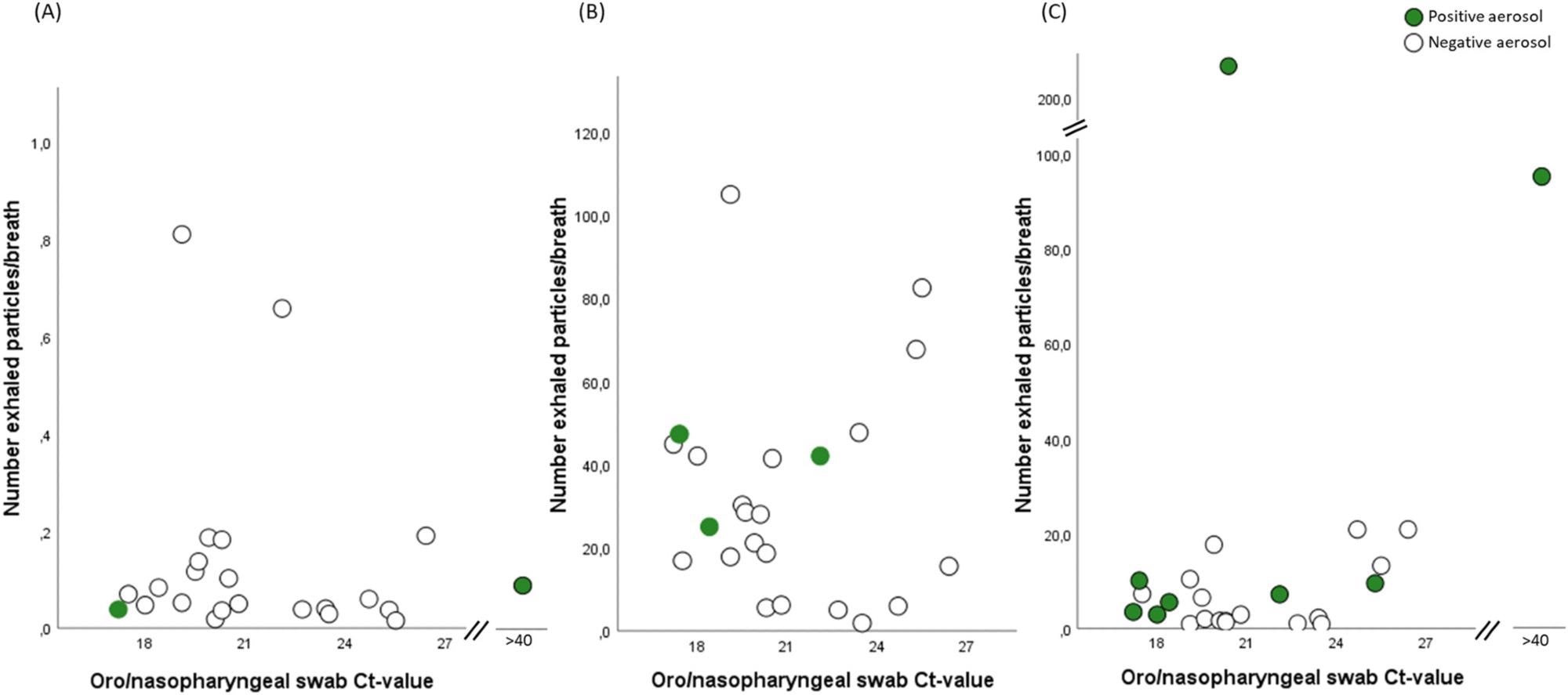 Number of exhaled particles/breath collected at (A) normal breathing, (B) airway opening and at (C) cough, in comparison with viral load in oro/nasopharyngeal swab samples, in subjects with coronavirus disease 2019 (COVID-19) (n = 25). Number of exhaled particles is expressed as n * 1,000 (kn) per breath. Subjects with COVID-19 and with a positive aerosol sample but with a negative reverse transcription real-time polymerase chain reaction (RT-PCR) from oro/nasopharyngeal swab samples are here presented with a cycle threshold (Ct) value above 40. Particle data are missing in one case in (A)
Number of exhaled particles/breath collected at (A) normal breathing, (B) airway opening and at (C) cough, in comparison with viral load in oro/nasopharyngeal swab samples, in subjects with coronavirus disease 2019 (COVID-19) (n = 25). Number of exhaled particles is expressed as n * 1,000 (kn) per breath. Subjects with COVID-19 and with a positive aerosol sample but with a negative reverse transcription real-time polymerase chain reaction (RT-PCR) from oro/nasopharyngeal swab samples are here presented with a cycle threshold (Ct) value above 40. Particle data are missing in one case in (A)
There was no overlap between SARS-CoV-2-positive aerosols during normal breathing and airway opening maneuver using the PExA method or between BE and PExA samples from 20 normal breaths. According to the authors, the low amounts of sampled aerosol particles during normal breathing could explain the low detection rate.
The presence of viral RNA in aerosol detected with PExA was mostly found on the impactor stage sampling particles of size less than 5 μm which is in line with previous findings and was also supported by the recent findings showing SARS-CoV-2 RNA is abundant in aerosols with particle sizes less than 5 μm.
The researchers found that although SARS-CoV-2 was present in lower, upper, and central airways, most of its deleterious effects may be exerted in the terminal bronchioles and alveoli. Thus, positive aerosols in airway opening maneuver samples may highlight SARS-CoV-2 dissemination to the distal airways early in the course of the disease. However, contamination from the upper airways during the airway opening maneuver cannot be fully ruled out.
Conclusion
The study findings show that SARS-CoV-2 RNA can be detected in exhaled aerosol samples during breathing and coughing early in the COVID-19 disease course. Furthermore, the viral RNA detection in aerosols seemed to be independent of the exhaled number of particles and the viral load in the upper airway swab.
The results show that only a minimal amount of aerosol is needed to detect SARS-CoV-2 RNA under some conditions. The possibility of detecting the virus in exhaled breath depends on the sampling method, the breathing pattern, and the amount of virus present on the surface where the aerosol particles are formed.
According to the authors, more studies need to explore further the infectious potential of the viral load detected in aerosols of subjects with COVID-19.