Soon after the emergence of the newest severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Omicron (B.1.1.529) variant, there has been a rapid increase in coronavirus disease 2019 (COVID-19) cases around the world. While the global scenario suggests a reduced severity of Omicron infections, the scale of these new COVID-19 cases points to the likelihood of increased hospitalizations and deaths in people living with comorbidities and weak immune systems.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
To resolve the uncertainties associated with prospects of Omicron-associated COVID-19, researchers in the United Kingdom recently conducted a cohort study in the residents of long-term care facilities (LTCF), representing the most disease susceptible section of the society, who tested positive for SARS-CoV-2.
The current study, which was published on the preprint server medRxiv*, has found a markedly reduced risk of hospitalizations and deaths in LTCF residents infected with Omicron compared to previous SARS-CoV-2 variants. In addition, none of the residents with a history of COVID-19 or who had received a vaccine booster dose required hospitalization during the study period.
Taken together, these findings suggest that the current Omicron wave of infections is unlikely to result in any surge in the serious disease in LTCF populations, with high levels of natural or vaccine-induced immunity.
Background
The SARS-CoV-2 Omicron variant, which was first detected in November 2021, contains approximately 30 mutations in the spike gene. As the most heavily mutated spike protein of SARS-CoV-2 to date, researchers have raised concerns on the effectiveness of available vaccines and therapeutic antibodies, which primarily target the spike protein.
As a highly transmissible variant with immune escape potential, Omicron currently accounts for approximately 98% of sequenced samples in the U.K. and the United States and more than 60% of sequenced samples throughout the globe.
Previous studies have suggested a lower risk of severe outcomes following infection due to Omicron in the general population. However, only limited reports are available on the outcomes in older populations with high rates of comorbidities, such as the residents of LTCFs who have been disproportionately affected by the pandemic.
Approximately 50% of LTCF residents are aged 85 years or older and have high levels of comorbidities. In the U.K., coinciding with the emergence of the Omicron variant, there has been a rapid increase in the number of outbreaks in LTCFs since December 2021, despite the fact that 85% of the LTCF residents have already received the third dose of their COVID-19 vaccine.
Our study provides important insights into the risk of severe outcomes in LTCF residents, who are frequently excluded from research studies, and have experienced among the highest rates of SARS-CoV-2 related morbidity and mortality.”
About the study
The cohort study included LTCF residents with a median age of 84.6 years who tested positive for SARS-CoV-2 between September 1, 2021, and January 17, 2022. Based on the timing of the first Omicron case in the data set, the study period was divided into Pre-Omicron (September 1, 2021, to December 12, 2021, when Delta variant was predominant) and Omicron-dominant (December 13, 2021, to January 17, 2022) periods.
The primary outcome of hospital admission within 14 days following a SARS-CoV-2 positive test. Comparatively, the secondary outcome of mortality was reported within 28 days following a positive test. Both primary and secondary outcomes were compared between the two study periods.
A subset of samples was confirmed for lineage through sequencing; however, in the event that sequencing was not available, quantitative polymerase chain reaction (qPCR) Cycle threshold (Ct) values were used to identify S-Gene Target Failure (SGTF).
SGTF is a reliable marker of the SARS-CoV-2 Omicron variant. The comparison of the risk of hospital admissions was repeated in this sub-cohort of residents with confirmed or probable Omicron or Delta infections.
The effect of multivariates such as sex, primary vaccine course, booster status, or age on the comparison of the risk of hospitalization between pre-Omicron and Omicron periods was also investigated.
Omicron-dominant period was associated with a major surge in cases
A total of 1,639 new SARS-CoV-2 cases were detected in 246 LTCFs during the study period, with 75.7% of cases diagnosed in the Omicron-dominant period and only 24.3% cases diagnosed before this period.
Of the total infected residents, 10.5% had evidence of past infection. However, none of these residents were admitted to the hospital, which suggests that naturally induced immunity still provided some degree of protection against the development of severe disease.
Lower hospitalizations in Omicron dominant period
The incidence of hospital admission following infection was lower in individuals infected in the Omicron period at 4.01% as compared to the pre-Omicron period hospitalization rate of 10.80%. The unadjusted hazard ratio (HR) for hospitalization following diagnosis in the Omicron period compared to the pre-Omicron period was 0.35.
The same pattern of reduced risk of hospital admission in the Omicron- versus Delta-dominated period was seen in residents, irrespective of whether they had received a primary course of SARS-CoV-2 vaccine or remained unvaccinated. As compared to those who had not received a vaccine booster dose, residents who received a booster before their diagnosis experienced a reduced risk of hospitalization in the Omicron period.
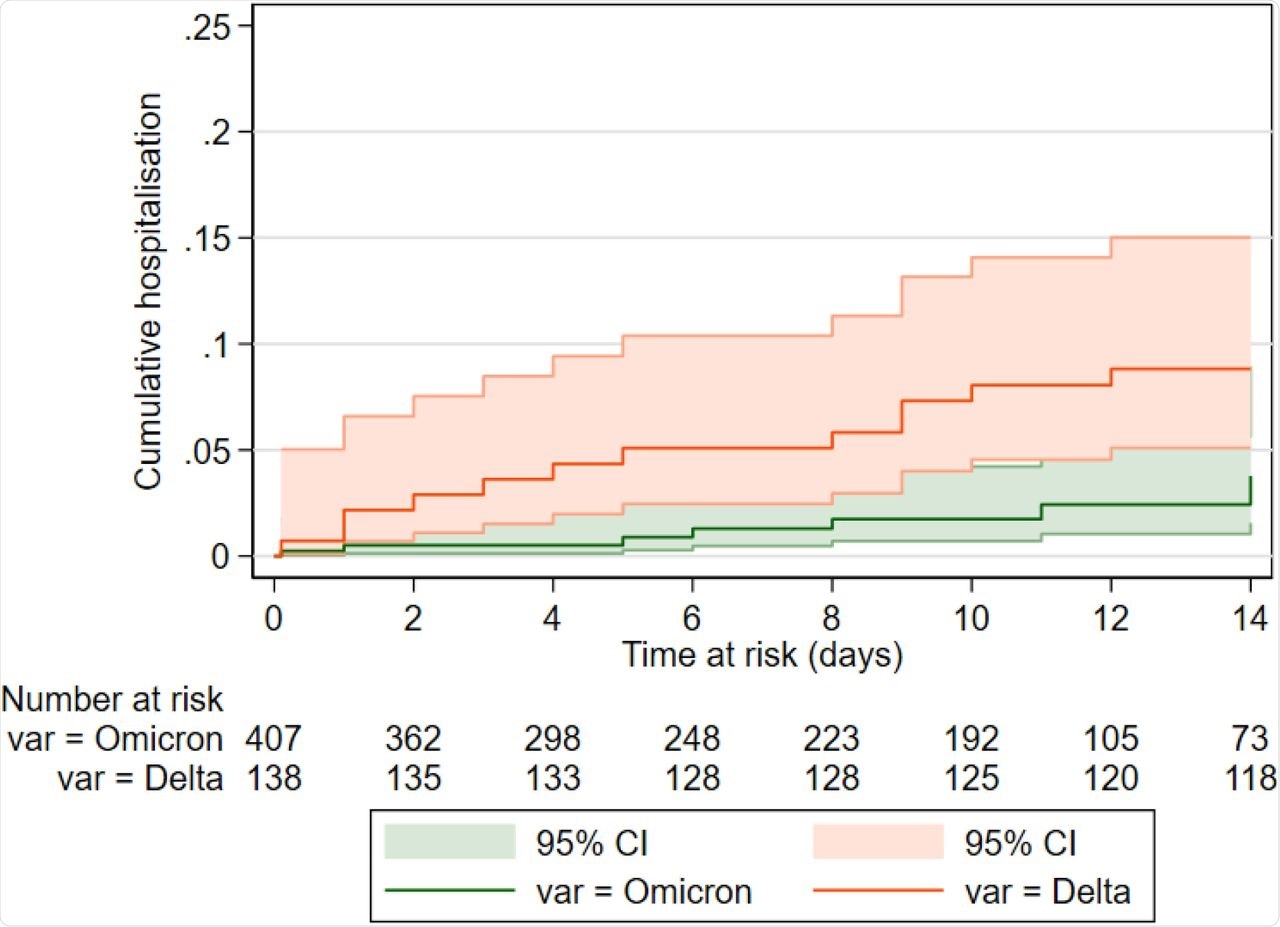
The findings from the Delta- and Omicron-dominated periods were matched with the sub-cohort of 545 residents with 138 confirmed/probable Delta cases and 407 confirmed/probable Omicron infections based on sequencing or SGTF. The proportion of residents admitted with Omicron infection was lower at 3.77% as compared to that with Delta of 8.82%.
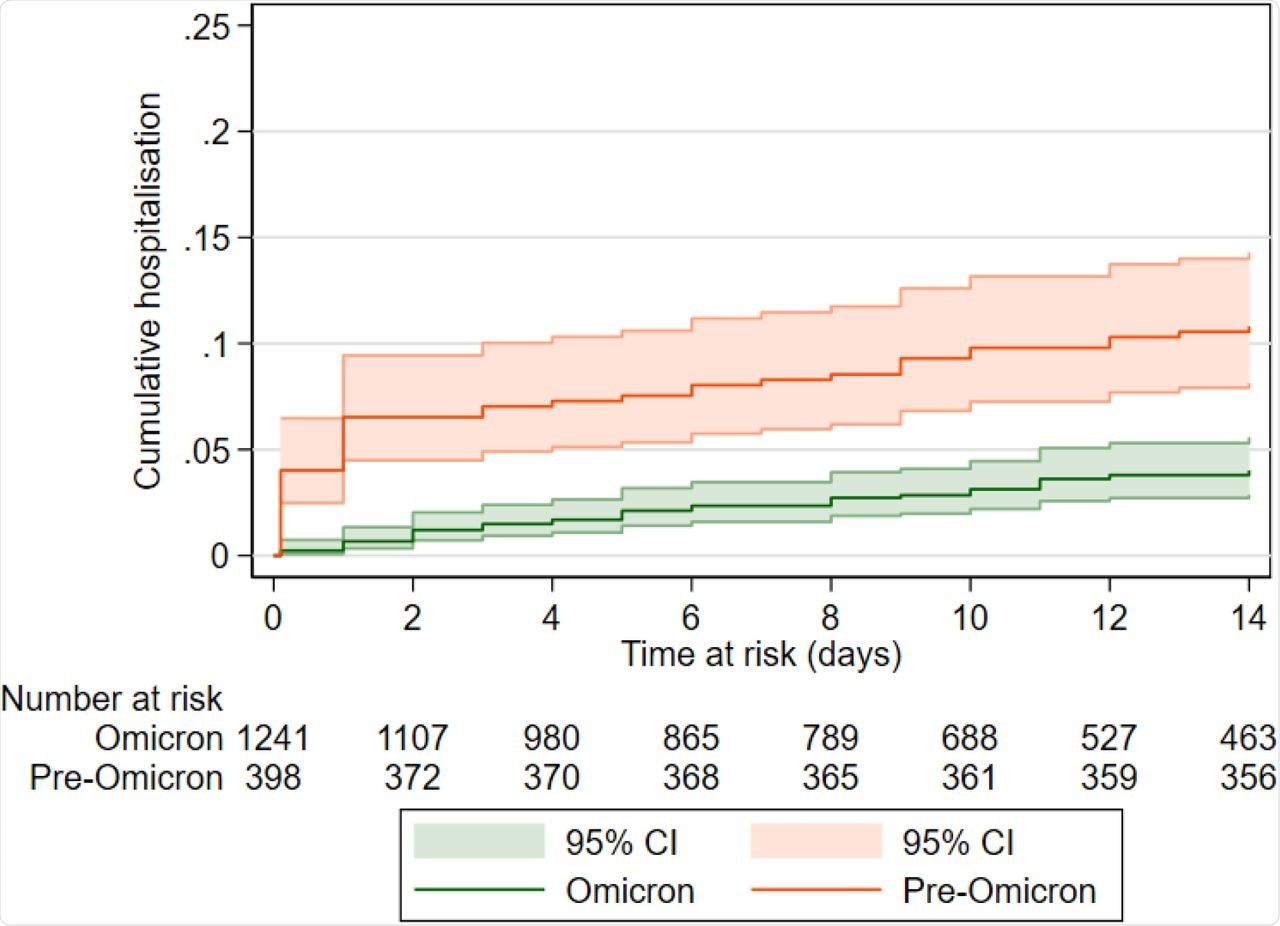
Kaplan Meier curve comparing the cumulative incidence of hospital admission in the 14 days following a positive PCR or LFD test in the pre-Omicron (September 1, 2021 - December 12, 2021) and Omicron periods (December 13, 2021 - January 14, 2022), p<0.0001. Participants who are not hospitalised are censored at the earliest of 14 days following test date or January 14, 2022.
Reduced risk of death during the Omicron-dominant period
The researchers of the current study observed a reduced risk of death within 28 days of a new SARS-CoV-2 diagnosis in the Omicron-dominant period of 1.1 deaths for 1,000 person-days as compared to the Delta-dominant period of 3.8 deaths for 1,000 person-days. Similarly, this finding suggests a reduced disease severity associated with Omicron infections.
Cumulative mortality in 28 days following SARS-CoV-2 test in the pre-Omicron and Omicron period (p<0.0001), between September 1, 2021 and January 7, 2022. Participants who do not reach the outcome are censored at the earliest of 28 days following the test date or January 7, 2022.
Overall, the markedly decreased severity combined with high vaccination uptake and prior natural infection can be expected to significantly limit the impact of the current wave of Omicron infections on hospitalizations and deaths in residents of LTCFs.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Krutikov, M., Stirrup, O., Nacer-Laidi, H., et al. (2022) Severe outcomes in residents of Long Term Care Facilities following infection with SARS-CoV-2 Omicron variant (VIVALDI study). medRxiv. doi:10.1101/2022.01.21.22269605, https://www.medrxiv.org/content/10.1101/2022.01.21.22269605v1
- Peer reviewed and published scientific report.
Krutikov, Maria, Oliver Stirrup, Hadjer Nacer-Laidi, Borscha Azmi, Chris R Fuller, Gokhan Tut, Tom Palmer, et al. 2022. “Outcomes of SARS-CoV-2 Omicron Infection in Residents of Long-Term Care Facilities in England (VIVALDI): A Prospective, Cohort Study.” The Lancet Healthy Longevity 3 (5): e347–55. https://doi.org/10.1016/s2666-7568(22)00093-9. https://www.thelancet.com/journals/lanhl/article/PIIS2666-7568(22)00093-9.