
 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Background
The most recent global surge of COVID-19 cases, which is driven by the emergence of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Omicron variant, has once again strained public health systems. The Omicron (B.1.1.529) variant was first detected and reported to the World Health Organization (WHO) on November 24, 2021, by South African researchers.
Since its original discovery, over 30 mutations in the B.1.1.529 variant have been reported, a majority of which are present within the spike (S) protein that is critical for host cell entry. The alarming number of mutated sites within the S protein is largely responsible for the rapid spread of the Omicron characterized by increased binding affinity to host receptors and immune-evasive traits.
In the United Kingdom (U.K.), the first Omicron case was confirmed on November 27, 2021. Within a month, over 159,900 Omicron cases were identified in the U.K.
This record number of cases raised alarms over existing self-isolation policies and their impact on labor shortages, supply chain constraints, and economic effects. As a result, there was a growing need to address concerns to avert adverse effects on the economy.
Previously, LFDs have been used to observe the status of infected individuals to tailor the self-isolation period based on LFD test results.
About the study
In the current study, the researchers extrapolated their previous findings and analyzed potential policies aimed at mitigating the self-isolation period. The authors discuss and compare the possible risks and benefits of using a single negative LFD test with multiple consecutive negative LFD results to allow early release from isolation.
The model employed in the current study simulates 500,000 individuals with an assumption that all of them were infected with SARS-CoV-2 at some point. To this end, a random infectious period (tinf in days) is assigned to each individual sampled from a gamma distribution.
At time (t) = 0, individuals were considered positive for COVID-19, either with testing or symptomatic development and commenced their pre-defined self-isolation period. The time point of t = 0 coincided with the start of the infectious period.
Infected individuals were permitted to regularly take LFD tests at the 24-hour interval following an initial isolation burn-in period for up to a maximum of ten days after the onset of the infectious period (t = 0). For each LFD test taken on day ti, the individual was considered infectious if ti < tinf and recovered or no longer infectious if ti ≥ tinf.
The excess time spent in isolation when the individuals were no longer infectious (ti – tinf) was calculated, as well as the time they remained infectious (tinf - ti) after release.
Study findings
Several scenarios were generated where the initial burn-in period was five days that required a single negative LFD result as compared to four and three days of burn-in. These latter days required two and three consecutive LFD negative results to be released early from isolation, respectively.
The researchers found that an individual in five days of isolation before taking LFD tests would, on average, be infectious for 20.4 hours after release with 40 excess hours spent in isolation. An individual with ten days of isolation would remain infectious for 4.4 hours, with 119.9 hours spent excess in isolation.
For individuals who received three consecutive negative tests after spending a minimum of three days in isolation before taking LFD tests, the infectious period after release was 4.4 hours, with 50.5 hours spent in excess during isolation.
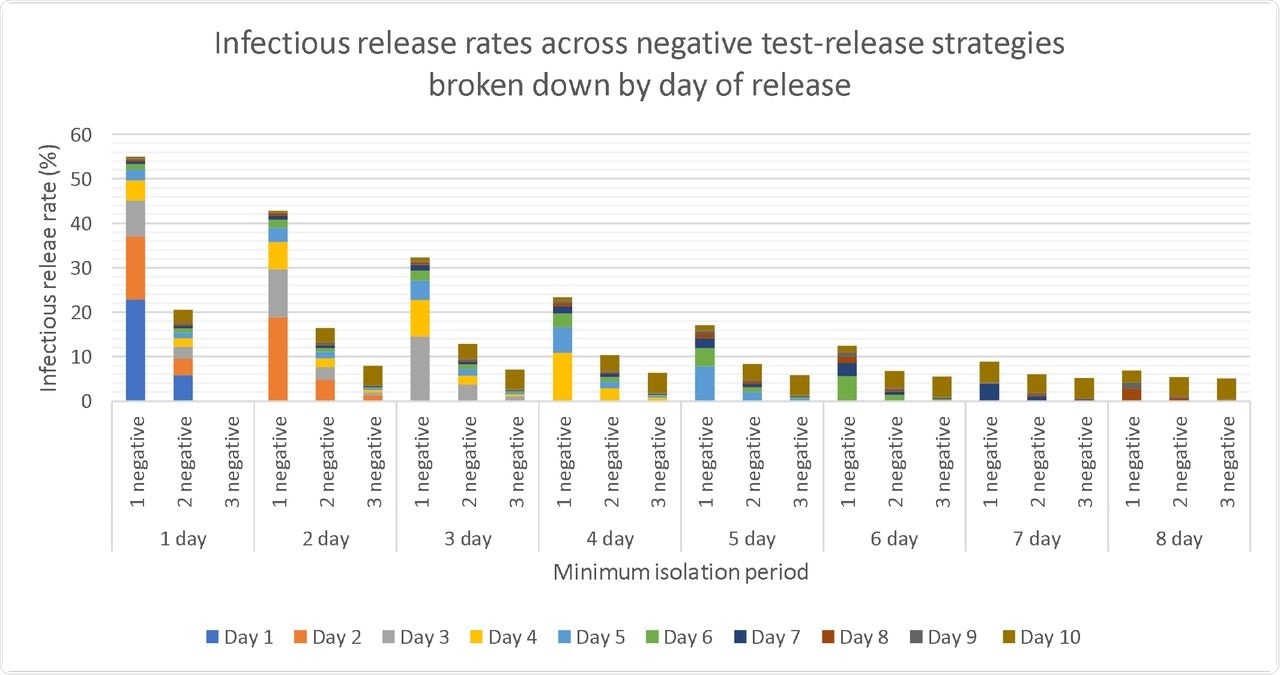
Plots of average release rates at which model reported infectious individuals being released early for each considered scenarios, broken down by day on which infectious individuals are released.
Conclusions
The findings presented in the study reveal that with this approach of individuals released with a single LFD negative result after five days of the minimum isolation period, the release of infectious individuals could decline by 46%.
This was further decreased with multiple tests, which showed a 74% and 81.4% decline in infectious releases for two and three consecutive negative LFD tests, respectively. Moreover, a shorter minimum isolation period before LFD tests was associated with a higher proportion of early infectious releases. Nonetheless, multiple negative tests decreased this effect.
The current work demonstrates the use of modeling to implement a tailored self-isolation period based on negative LFD test results. Furthermore, this approach demonstrated that excess time can be reduced during isolation; therefore, the number of infectious individuals released early from isolation could be decreased.
Multiple testing was shown to be more beneficial than a single negative LFD test. As a result, the researchers proposed that two consecutive negative LFD results be implemented for planning a personalized self-isolation period considering the modeling results and cost of LFD testing.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.