The prevalence of inflammatory airway diseases such as lung cancer, chronic obstructive pulmonary disease (COPD) and asthma is on the rise internationally, placing strain on health systems around the world. Lung cancer is the leading cause of death of all cancers. Asthma and COPD, while less often deadly, can have long-lasting and significant effects on patients’ quality of life. For each of these diseases, diagnostic methods are both costly and invasive.
Volatile organic compounds (VOCs) on exhaled breath hold the potential for cheaper, faster, and non-invasive screening, for both early detection (in the case of cancer) and ongoing monitoring (in the cases of COPD and asthma). However, lung disease diagnosis using breath VOCs is challenging and no breath VOC tests are currently clinically available. In this review key studies from 2010-2019 have been evaluated, in order to demonstrate the progress made in this field. The selection of studies was systematically reduced to 60 qualifying publications. This included 33 clinical studies related to lung cancer, 14 associated with COPD, and 10 with asthma. The remaining three focused on differentiating between multiple of these conditions based on detected VOCs. 30 studies reported VOCs as biomarkers, accounting for a total of 146 molecular features. A number of different analytical platforms were used across the studies. It was noted that “GC-MS remains the gold standard for VOC analysis in many fields” with “high potential for both identification and quantification of unknown components”.
Breath samples can contain more than 1,000 compounds from both endogenous and exogenous sources. Endogenous compounds can originate from all over the body and are often products of metabolism. Selecting the right VOCs to use in a breath test for a given disease, needs to be based on an in-depth knowledge of the underlying biology associated with the disease. As conditions characterized by chronic inflammation, lung cancer, COPD and asthma have high potential for diagnosis and disease monitoring via exhaled VOCs linked to inflammation.
A number of limitations and challenges have prevented the development of breath tests for these inflammatory lung conditions thus far. They include, according to the authors of this review, a lack of standardization of sampling and analytical methods across studies, inconsistent use of controls, small patient cohorts, and more. All these factors have together led to a lack of reproducibility between studies.
Comparing prospective biomarkers across studies
Across 21 of the studies related to lung cancer that were considered, 83 different biomarkers were proposed, with only 31 reported by at least two studies. 2-butanone, was the most popular suggestion, put forward by six studies. Xylene was labelled as a prospective biomarker in five studies and nonanal, 2-pentanone, 3-hydroxy-2-butanone and hexanal appeared in four studies.
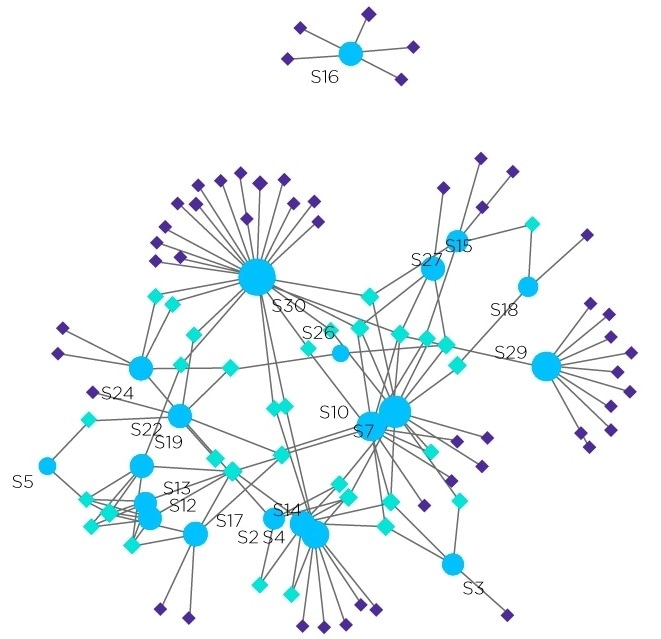
Figure 1. Network analyses of lung cancer studies distribution based on detected volatiles, where circles represent studies, pale diamonds represent the common VOCs and darker diamonds depict the uncommon VOCs. Image Credit: Owlstone Medical Ltd
Commonality between the VOC biomarkers proposed for COPD and asthma, across the studies considered, was even worse, with no common compounds reported for asthma. Six studies reported biomarker identification for COPD, with hexanal, in common between three of those studies and five other VOCs mentioned in two studies.
The compounds that were common between lung cancer studies and COPD studies were largely common for asthma as well. This suggests that these VOCs are not markers for a given lung condition, but rather of inflammatory airway disease more generally. This corroborates other studies that have previously linked the chemical families of some of these VOCs with particular inflammation processes, that could be relevant across multiple disease groups. The specific contexts of a disease can shape the metabolic processes involved in inflammation and therefore the resulting VOCs, so even though inflammation is a common component of diseases throughout the body inflammation-associated VOCs still hold great potential diagnostically.
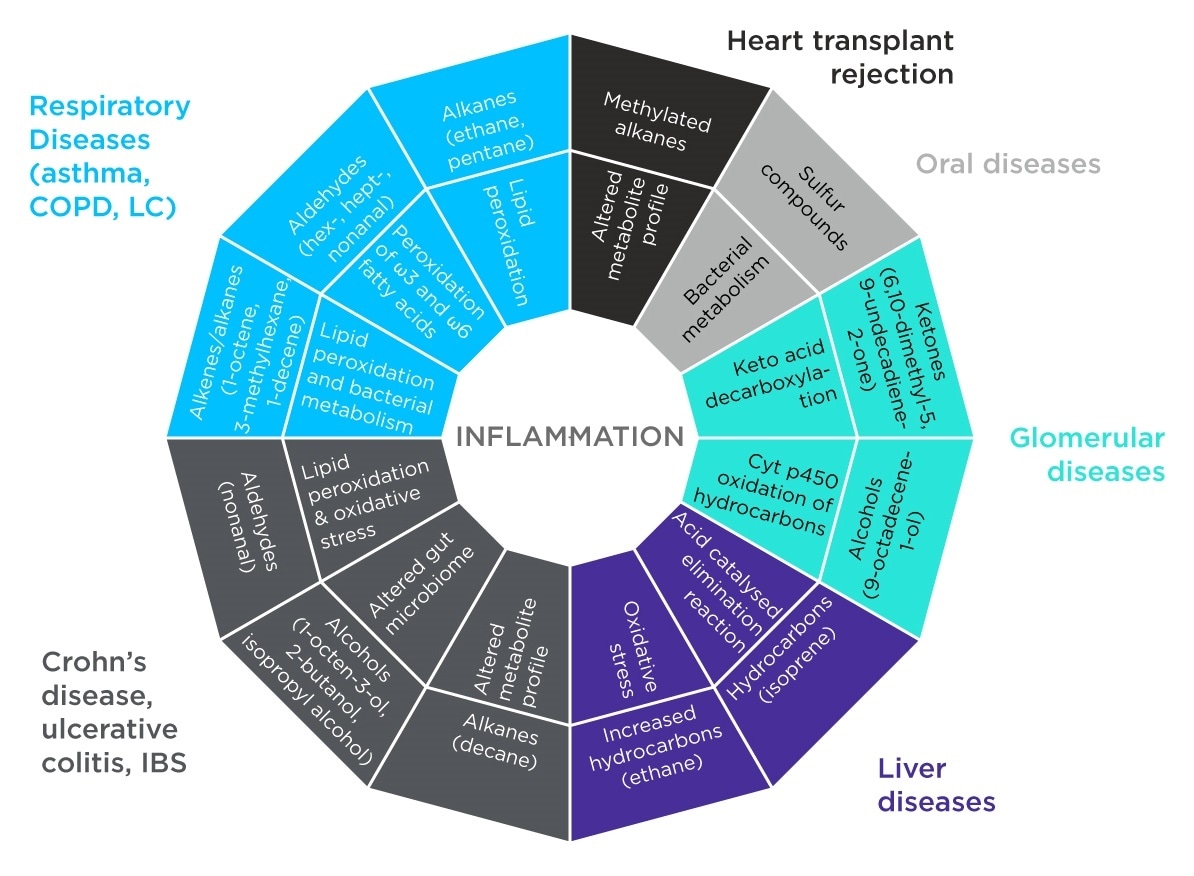
Figure 2. VOCs Resulting from Inflammation Processes. Image Credit: Owlstone Medical Ltd
All this suggests that the field of breath research would greatly benefit from a more standardized approach to sampling, analysis and data processing, that would enable a more consistent comparison of biomarkers across studies. This is more likely to lead to the discovery of breath biomarkers that can provide clinically relevant information. The review paper specifically mentions the ReCIVA Breath Sampler and the CASPER Portable Air Supply as being devices that have been designed with standardized sampling in mind.
Conclusions
Promising findings have been reported, in the last decade, both relating to tests that discriminate between lung diseases and that provide a predictive diagnosis, however breath tests for respiratory diseases are still a little way off being available for clinical use. In the short term the study predicts that “analytical instrumentation will be used in small point of care studies to confirm or deny the possibility of certain respiratory conditions. Based on this first diagnosis the subjects may then be sent for a more complex and confirmatory diagnosis”.
Read the original article here: www.owlstonemedical.com/science-technology/research-case-studies/biomarkers-inflammatory-diseases/