Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) first emerged at the end of 2019 in Wuhan, China, and transpired into the ongoing coronavirus disease 2019 (COVID-19) pandemic – which has affected nations around the world and has claimed more than 5.78 million lives globally. Numerous RNA and DNA-based vaccines have been approved for emergency use and most countries have propagated and implemented mass vaccinations.
The antibody responses and immunological memory induced by vaccines have proven highly effective against hospitalization and mortality. However, their long-term efficacy is yet to be ascertained against ever-emerging SARS-CoV-2 variants.
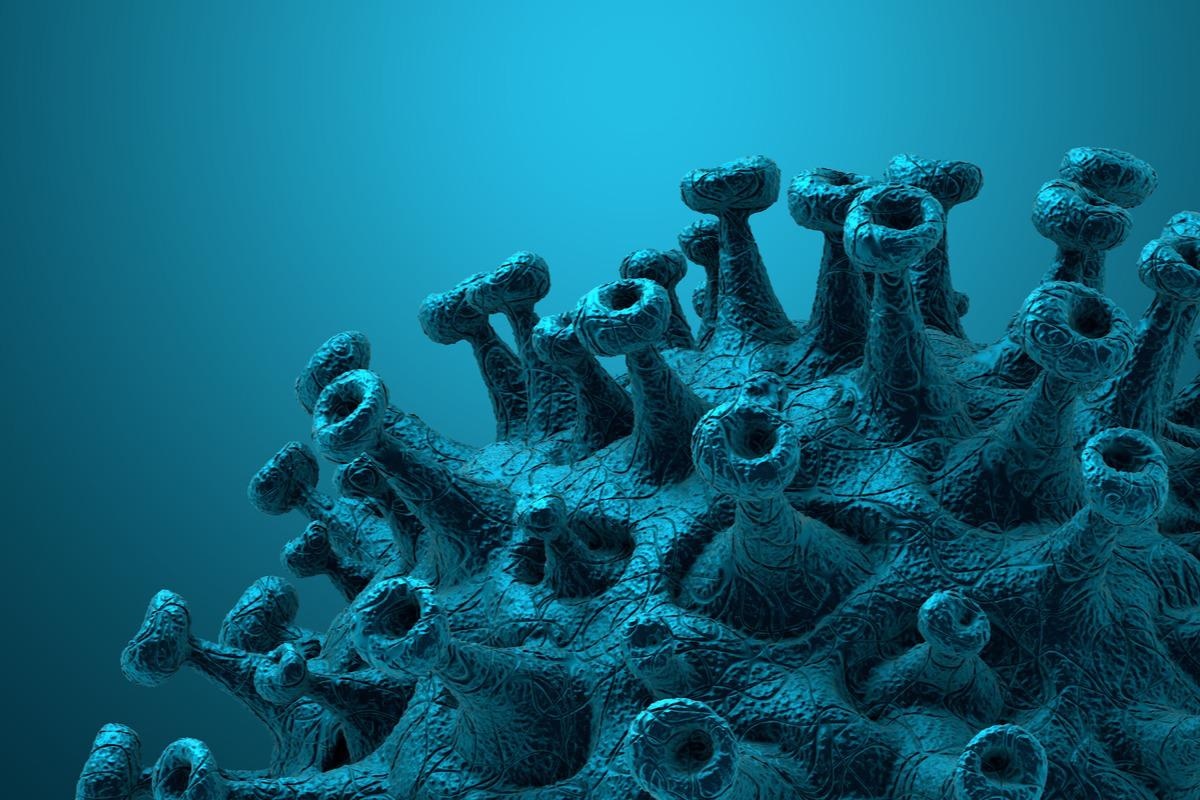 Study: A Feasible Alternative Strategy Targeting Furin Disrupts SARS-CoV-2 Infection Cycle. Image Credit: CROCOTHERY/Shutterstock
Study: A Feasible Alternative Strategy Targeting Furin Disrupts SARS-CoV-2 Infection Cycle. Image Credit: CROCOTHERY/Shutterstock
Background
SARS-CoV-2 infects through entry into the lung cells, which is dependent on spike receptor-binding domain (RBD) interactions with angiotensin-Converting Enzyme 2 (ACE2). Unlike severe acute respiratory syndrome coronavirus (SARS-CoV), the SARS-CoV-2 spike protein contains an arginine-rich site (S1/S2)—between attachment (S1) and fusion (S2) domains—the cleavage of which by host cellular furin protease is crucial in efficient host cell membrane fusion during the transmission chain.
Experimental studies have revealed that the solvent-exposed furin cleaved region (S1/S2) interacts with additional surface receptors to enable viral cellular entry and heightens disease pathogenicity. Hence, an alternative strategy to obstruct the SARS-CoV-2 infection cycle could be by selectively targeting furin in virus-producing cells.
The study
A recent study published in Microbiology Spectrum was based on the hypothesis that competitively inhibiting cellular furin and selectively targeting SARS-CoV-2 in the infected viral-producing cells is critical for therapeutic specificity.
Here, a spike targeting immunoglobulin (Ig)G1-Fc-based design was engineered to selectively compete with early, late, recycling endosomal, and cell surface enriched furin protease function at the site of potential spike-trafficking, processing and incorporation into the virus. This approach that competitively inhibits furin through engineered and flexibly linked Fc-extended peptide beyond the CH3 domain, was termed FuG1 – an anti-spike IgG1.
The study described a targeted antibody-based plug-and-play FuG1 strategy that directly interferes with the furin-dependent proteolytic mechanism of spike cleavage and activation apart from destabilizing the full-length spike protein.
Organelle fractionation studies strengthen the furin-mediated spike processing and viral egress via the deacidified lysosomal/endosomal system. It was speculated that FuG1 strategy-mediated targeting of furin likely operates outside the trans-Golgi-network (TGN).
Here, the engineered furin disrupter – FuG1, was assessed in human lung tissue cells. The results demonstrated that adding the furin disruptor peptide did not impede the function of the antibody or its ability to bind to the SARS-CoV-2 spike. FuG1 significantly interfered with the spike cleavage at furin sites. In addition, FuG1 impacted the overall stability of the SARS-CoV-2 spike protein, which renders the virus infectious and plays a critical role in the transmissibility of the virus.
Considering the site of spike furin cleavage and the SARS-CoV-2 exit is inconsistent, these experiments uncovered novel mechanisms of proteolytic processing of the spike protein. Hence, it was found that proteolytic processing does not occur in the constitutive secretory pathway.
Additionally, blockade of furin-mediated cleavage of the spike protein was evident for membrane fusion activation and virus host-cell entry function. These findings introduced alternate applicability of the host protease system in targeting SARS-CoV-2, as well as future coronaviridae family members, to gain cellular entry and subsequent chain of infections by exploiting the host protease system.
Conclusion
Since the furin-mediated cleavage of the SARS-CoV-2 spike protein—mediated by host cells—is essential for viral entry and for the chain of the infection cycle, the strategy described here of an antibody Fc-conjugated furin competing peptide is of importance. If the spike protein mutations do not interfere with the Fc-conjugated antibody's epitope, the above-mentioned furin competing strategy can be employed in designing a broad spectrum of targets to inhibit the production of more transmissible SARS-CoV-2 variants of concern.
Furthermore, the proposed approach offers a plug-and-play option that can target other potentially deadly viruses that utilize secretory pathway-independent host protease machinery for cellular entry for infection.