
 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Introduction
The ongoing COVID-19 pandemic has created repeated spikes of cases and hospitalizations, including deaths, over the past two years. The mortality rate varied from country to country, with the highest being about 20% in Yemen, while Burundi reported a COVID-19 mortality rate of 0.1%.
Children and young people appear to be less vulnerable to severe COVID-19 following SARS-CoV-2 infection. The mortality rate in this population is relatively low at less than 1% in several countries including New Zealand, Maldives, Qatar, and Singapore. Notably, many people never test positive for SARS-CoV-2, despite having close and prolonged contact with a known infected individual, and half of those who test positive are asymptomatic.
The explanation for these puzzling findings may lie in the immune response elicited by the measles-mumps-rubella (MMR) vaccine, which, like several other vaccines including the poliovirus, Hemophilus influenza type B, and pneumococcal vaccines may resist SARS-CoV-2 through a nonspecific immune response. The current study seeks to distinguish the immune response to the MMR vaccine from other vaccine responses as the primary vaccine that confers SARS-CoV-2 cross-immunity.
The MMR vaccine was first offered in 1971; however, two doses of this vaccine were given only from 1979 onwards. Thus, most individuals aged 50 years or above would not have received the vaccine at all. This may provide an additional explanation for the increased mortality associated with COVID-19 among people above the age of 50.
Individuals between the ages of 42 and 49 years have likely received a single dose of the MMR vaccine, while those aged 41 or less likely received two doses. This could be why the death rate from COVID-19 is somewhat greater in the former group as compared to the latter.
Italy, France, and the United Kingdom have some of the lowest COVID-19 mortality rates, all of which have recently set up mass vaccination programs. The current study is based in Iran, which carried out a national campaign to vaccinate people aged five to 25 years with the MMR vaccine.
Study findings
A total of 46 patients with a confirmed positive test for COVID-19 were selected for the current study, of whom 36 were from the COVID-19 ward and the remaining from the intensive care unit (ICU). Of the 36 study participants, just over 40% were male. About 50% of the study participants had other medical conditions like hypertension, heart failure, or diabetes.
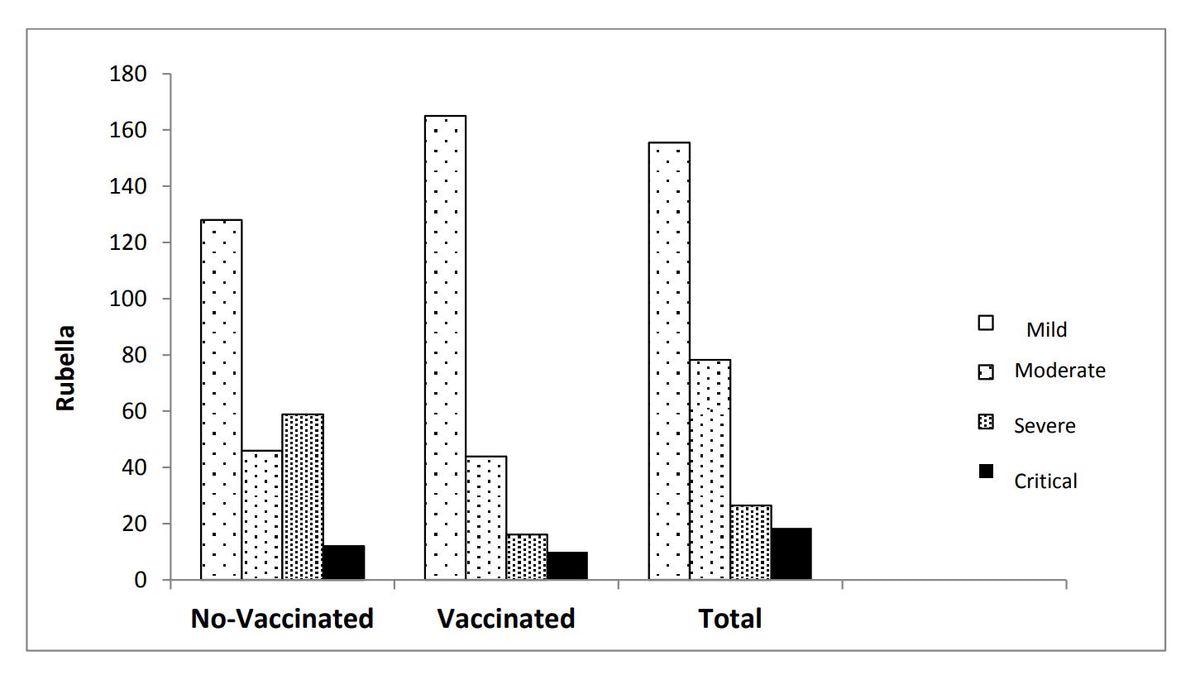
Distribution of rubella IGG level, based on different severities of the COVID-19 by vaccinated and unvaccinated groups
Common presenting symptoms of COVID-19 were cough, difficulty breathing, and weakness. About 75% of the patients required supplemental oxygen, whereas only a few patients required intubation or mechanical ventilation.
About 50% of the patients had been vaccinated against COVID-19 and less than one in seven had received the third booster dose. A variety of COVID-19 vaccines were recorded, including that from Sinopharm, Gamaleya, Oxford-AstraZeneca, and CoVIran vaccines. Severe disease was recorded in half of the patients, while less than 10% had critical disease. One of the patients in this study did not survive.
Mean rubella antibody titers of 77 AU/ml were measured within 48 hours of admission. The higher the rubella immunoglobulin G (IgG) titer, the less severe the condition of the COVID-19 patient was and the lower the SpO2.
Rubella IgG levels were not significantly different between COVID-19 vaccinated and unvaccinated people. However, in the vaccinated group, clinical severity was correlated with the rubella IgG titers, whereas no correlation was observed in the other group.
The median titers of rubella IgG differed in the groups aged 43 years or less as compared to those over the age of 43 years. Vaccination against COVID-19 and rubella IgG titers were interactive with respect to COVID-19 severity.
Implications
The current study demonstrates that high titers of rubella IgG are associated with less severe COVID-19. Although a history of COVID-19 vaccination was independent of rubella IgG levels, the presence of both was synchronous in reduced COVID-19 severity.
The large difference in rubella IgG titers in people aged 43 years or less and those above this age was about 100 units. The association of rubella IgG titers in those younger than 43 years of age with higher rubella IgG titers and milder COVID-19 is remarkable.
Recent work by other researchers originated the hypothesis that MMR vaccination on a large scale may be linked to fewer COVID-19 deaths. This could be due to cross-reactive antibodies elicited by MMR antigens that are similar to SARS-CoV-2 epitopes, as both vaccine viruses and SARS-CoV-2 possess glycoprotein spikes.
The measles vaccine virus is the most likely candidate, as some studies have reported that B-cell immunity triggered by measles vaccination is cross-reactive with SARS-CoV-2 antigens, thus causing a rise in the levels of measles IgG. The epithelial Fc receptor can also interact with the IgGs and traffick them into the cell to disrupt viral replication.
The nonspecific innate immune responses due to early childhood vaccination with MMR vaccines could be responsible for a rise in antiviral interferons and natural killer (NK) cells when faced with SARS-CoV-2. These responses could thus account for the singular protection observed in children below ten years of age against COVID-19.
In corroboration of this theory, only one of the 955 sailors aboard the USS Roosevelt who tested positive for SARS-CoV-2 was hospitalized. All sailors in the U.S. navy are vaccinated with MMR. In addition to MMR vaccination, natural exposure to the virus could act as a booster and thus maintain a high level of the rubella IgG.
Further research is required to establish this hypothesis in studies with a larger number of participants.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Sahebi, L., Hosseini, M., Abdollahi, A., et al. (2022). Does the Rubella Immunoglobulin G affect the severity of COVID-19? Rubella Immunoglobulin G and COVID-19. Research Square. doi:10.21203/rs.3.rs-1414903/v1. https://www.researchsquare.com/article/rs-1414903/v1.
- Peer reviewed and published scientific report.
Sahebi, Leyla, Mohsen Hosseini, Alireza Abdollahi, Nahid Farrokhzad, Samrand Fattah Ghazi, Farzaneh Samaei Noroozi, and Fereshteh Ghiasvand. 2022. “Does the Rubella Immunoglobulin G Affect the Severity of COVID- 19? .” BMC Microbiology 22 (1). https://doi.org/10.1186/s12866-022-02563-5. https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-022-02563-5.