While short-term lung damage has been reported in patients hospitalized with pneumonia caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), there is little data on the more chronic sequelae of this condition. A new research paper summarizes data from patients seen one year from discharge.
Both pneumonia and acute respiratory distress syndrome (ARDS) have been frequently found in COVID-19 and may lead to lung damage, including fibrosis. This is associated with short-term complications, observable at 3-6 months from discharge, though varying through a range of severity. For instance, some patients show mild impairment, but others may have exertional breathlessness.
The severity of the respiratory failure and the need for higher levels of respiratory support, in terms of intubation and mechanical ventilation, during the episode of pneumonia, are factors regulating the risk of sequelae involving the lungs. While short-term sequelae have been documented, some early research indicates that residual radiological abnormalities continue to show up on lung computed tomography (CT) at one year from pneumonia.
Findings included ground-glass opacities and fibrotic interstitial lung abnormalities (ILA), and traction bronchiectasis, though non-fibrotic ILA healed at least in part. In addition, lung diffusion studies showed impairment in over half of critically ill patients, and a third continued to have breathlessness at one year.
The current study, published in the journal Respiratory Research, looked at pulmonary sequelae in patients one year from discharge for COVID-19 hospitalized with pneumonia.
What Did the Study Show?
Over 300 patients with SARS-CoV-2 pneumonia were included in the study, of whom over 90% continued to be followed up to one year. About 60 patients, 140 patients, and 90 patients were on supplemental oxygen alone, continuous positive airway pressure (CPAP) ventilation, and invasive mechanical ventilation (IMV) respectively. No patient died during the second half of the study, but five required repeat admission for various causes.
Almost 70% of patients had no history of smoking, and approximately 80% had no or only one underlying medical condition. The incidence of pulmonary thromboembolism and deep vein thrombosis was low and comparable in both groups.
The lowest diffusion capacity for carbon monoxide (DLCO) was in the oxygen alone group and the least change in the CPAP group. DLCO improved in all groups between 6-12 months in CPAP and IMV groups by ~2.5%. Very few patients had restrictive lung changes, or obstructive patients, though in the latter four patients had either a history of or were current smokers, and one was asthmatic.
Other functions showed no difference between groups, with one in five patients showing a lower-than-expected distance walked. No group showed low oxygen desaturation or needed supplemental oxygen.
About 40% reported some breathlessness with mild exertion, while 34 patients reported they had to walk slowly or stop to catch their breath. When the 6- and 12-month follow-ups were compared, there was an increase in the reports of breathlessness in all groups, but not significant. None of the patients attended any rehabilitation program.
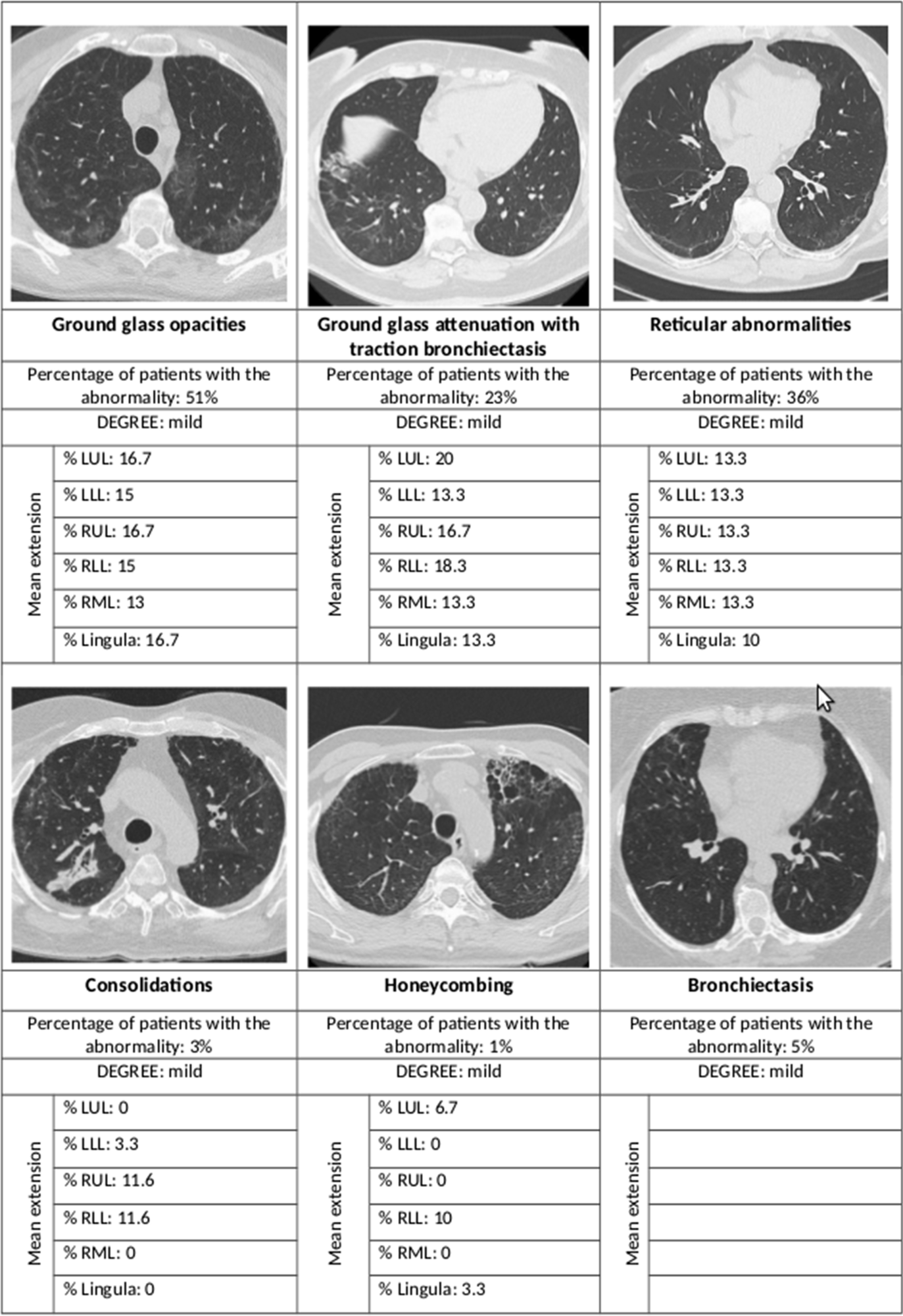
Summary of the main radiological abnormalities and their extension according to the lung lobe involved. LUL left upper lobe, LLL left lower lobe, RUL right upper lobe, RLL right lower lobe, RML right middle lobe
Radiological abnormalities were seen in 80% of the IMV patients, 65% of the CPAP, and 46% of the oxygen-only group. The risk was more than eight times higher in the first group and almost three times in the second group, compared to the last.
Most of the high-resolution CT (HRCT) scans showed interstitial lung changes; over half showed ground-glass opacities, over a third had reticular abnormalities, while less than 5% each showed consolidations and honeycombing. In 44% the ground glass opacities were accompanied by traction bronchiectasis or bronchiectasis.
Among patients with a normal DLCO, almost 60% had HRCT abnormalities, but when the DLCO was impaired, the proportion of radiological abnormalities went up to 77%. The same applied to ground-glass opacities, at 45% and 61%, respectively. Reticular abnormalities occurred in 28% and almost 50%, respectively.
What Are the Implications?
The findings show that fibrosis of the lung is an uncommon finding after SARS-CoV-2 pneumonia requiring hospitalization, with only 1% of patients showing this complication at 12 months from discharge. Most cases showed other mild interstitial results, mostly ground-glass opacities and reticular abnormalities, mainly within a single lobe and limited in extent.
This corroborates earlier reports but does not help to trace the source of the damage to the viral damage or because of changes in lung pressure or volume secondary to the IMV, even though the cystic alterations and pneumatocele formation seen in the latter case were not identified here.
Age is a definite risk factor for persistent radiological sequelae. DLCO impairment occurred more commonly among oxygen-only and IMV patients, but this could be due to selection bias. It is remarkable that “despite the mild entity of the functional sequelae, a consistent proportion of patients at 1-year from SARS-CoV-2 pneumonia still report exertional dyspnea (35%) with a worsening trend compared to the 6-month visit.”
The fact that this was independent of the severity of lung symptoms during hospitalization points to a common mechanism of lung damage rather than being entirely dependent on the severity of pneumonia. Such patients merit psychological support and rehabilitation in view of the debilitating effect of long Covid.
In fact, when these results as well as those of earlier researchers are compiled, it appears that careful follow-up should be provided to elderly patients with SARS-CoV-2 pneumonia requiring IMV to identify long-term pulmonary sequelae while not neglecting the other groups. Both DLCO and HRCT are useful in picking up pulmonary sequelae, which usually improve between 6 and 12 months.