The widespread use of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccines has played a critical role in curbing the mortality and morbidity caused by COVID-19. However, various reports of the waning efficacy of these vaccines have necessitated the identification and development of effective COVID-19 therapeutic methods.
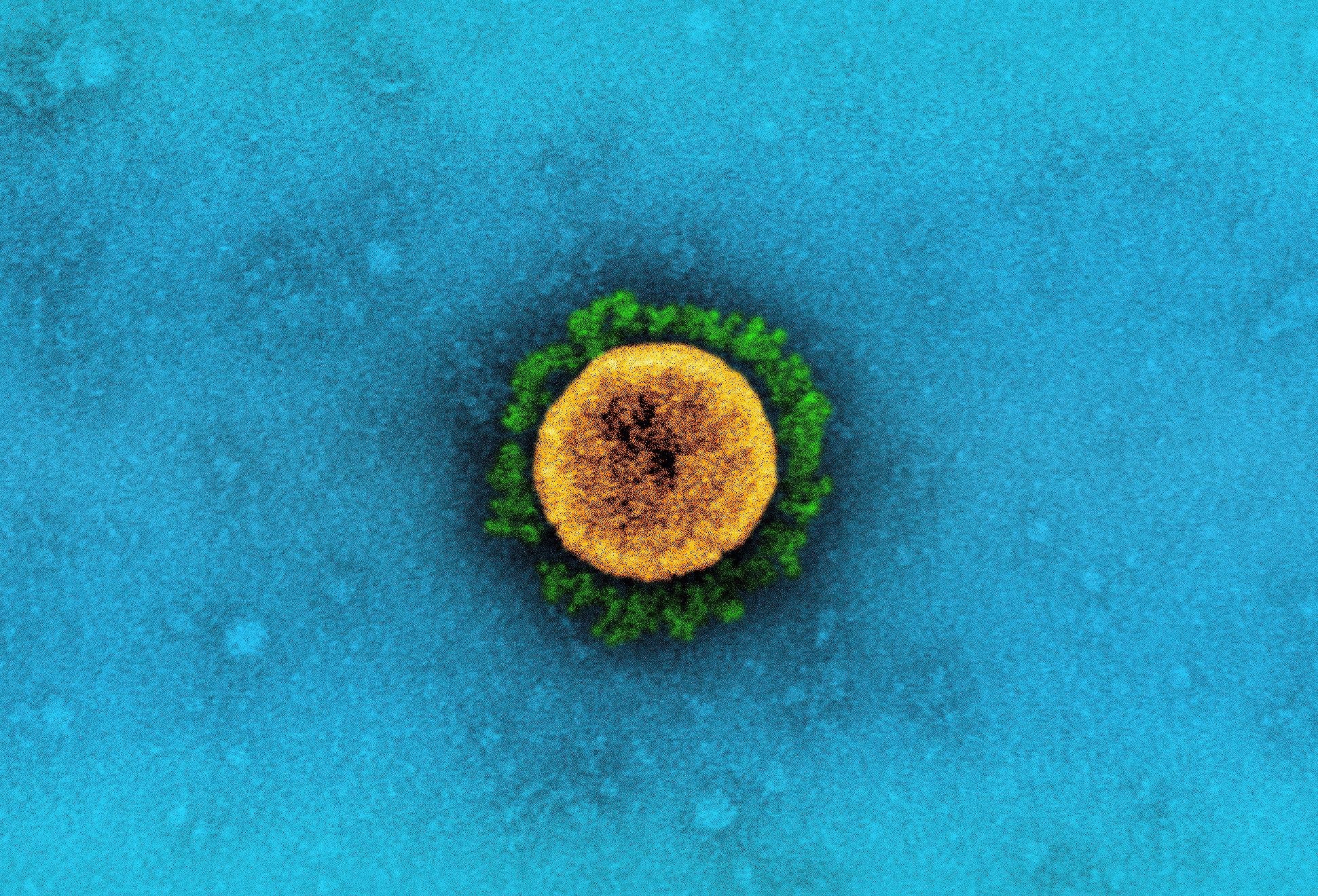 Study: Effect of Early Treatment with Ivermectin among Patients with Covid-19. Image Credit: NIAID
Study: Effect of Early Treatment with Ivermectin among Patients with Covid-19. Image Credit: NIAID
About the study
The present study evaluated the efficacy of ivermectin in preventing the progression of COVID-19, and related hospitalization among SARS-CoV-2 infected outpatients.
The team designed and conducted a double-blind, placebo-controlled, randomized, adaptive platform trial with local public health authorities in Brazil to test potential treatments using a master protocol. This master protocol defined the prospective decision criteria concerning the discontinuation of futile interventions, stopping due to the dominance of an intervention over a placebo, or the addition of new interventions.
The patients presented to an outpatient facility within seven days of symptom onset associated with COVID-19 and were aged 18 years or older. Also, eligible patients satisfied a minimum of one criterion concerning COVID-19 progression, like belonging to the age group of 50 years or older and reporting comorbidities including diabetes mellitus, hypertension, cardiovascular disease, smoking, lung disease, obesity, organ transplantation, chronic kidney disease, immunosuppressive therapy, cancer diagnosis within the last six months, or receipt of cancer-related chemotherapy.
The team tested the participants for SARS-CoV-2 via a rapid antigen test and collected data regarding their medical history, comorbidities, concomitant medications, previous COVID-19 exposure, and the patient’s clinical progression score according to the World Health Organization (WHO). The patients were also required to complete the patient-reported outcomes measurement information system (PROMIS) global-10 health scale. The recruited patients were randomly assigned to be administered with ivermectin or placebo between 23 March 2021 and 6 August 2021. The trial protocol prescribed administration of ivermectin and placebo for three days.
The study's primary outcome was (1) COVID-19-related hospitalization within 28 days since the trial began or (2) clinical worsening of COVID-19, which was defined as the clinical observation of the participant for more than six hours within 28 days since trial commencement.
The secondary outcomes of the study included (1) the clearance of SARS-CoV-2 as assessed by quantitative reverse transcription-polymerase chain reaction (qRT-PCR) on the third and seventh days of the trial, (2) hospitalization due to any cause, (3) the duration from symptom onset to hospitalization, (4) the duration of hospitalization, (5) the period till an emergency visit was required that lasted more than six hours, (6) the time to clinical recovery, (7) death from any cause, (8) the time to death (9) any mechanical ventilation required, (10) the number of days for which the mechanical ventilation was needed, and (11) the quality of life concerning health.
Results
The study findings showed that among the 10,467 outpatients screened for the trial, 679 patients were treated with ivermectin, and 679 patients received a placebo. The median age of both the cohorts was 49 years, with 58.2% of patients being females.
In the ivermectin-treated group, 14.7% of the patients showed a primary outcome event compared to 16.3% of patients in the placebo group. The most common event among the primary outcomes in the ivermectin population was hospitalization, as observed in 81.0% of the patients. Primary-outcome events were also observed after a median of five days after the trial began.
Furthermore, the team found no substantial differences between the ivermectin-treated and the placebo-treated groups concerning viral clearance on day 7. Also, no remarkable differences were observed between the two groups in the risk of hospital admission for any cause, the duration between recruitment and hospitalization, and the number of days spent hospitalized.
Moreover, the team noted no significant differences between the two groups regarding the time taken till clinical recovery, the risk of death, the number of days for which mechanical ventilation was required, or the time to death. Additionally, no differences were found between the ivermectin and placebo groups in the PROMIS global-10 score or the mental component score. In addition, no noteworthy inter-group differences were observed in the adverse events that occurred during the trial period.
Conclusion
The study findings showed that ivermectin treatment did not cause any significant differences in the number of COVID-19-related hospital admissions or the duration spent in emergency department observation among COVID-19-infected outpatients.
Journal reference:
- Effect of Early Treatment with Ivermectin among Patients with Covid-19. G. Reis, E.A.S.M. Silva, D.C.M. Silva, L. Thabane, A.C. Milagres, T.S. Ferreira, C.V.Q. dos Santos, V.H.S. Campos, A.M.R. Nogueira, A.P.F.G. de Almeida, E.D. Callegari, A.D.F. Neto, L.C.M. Savassi, M.I.C. Simplicio, L.B. Ribeiro, R. Oliveira, O. Harari, J.I. Forrest, H. Ruton, S. Sprague, P. McKay, C.M. Guo, K. Rowland-Yeo, G.H. Guyatt, D.R. Boulware, C.R. Rayner, and E.J. Mills. New England Journal of Medicine 2022, DOI: 10.1056/NEJMoa2115869, https://www.nejm.org/doi/full/10.1056/NEJMoa2115869