Vaccination against severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is critical to combat the COVID-19 pandemic. Recently, several reports have surfaced indicating autoimmune hepatitis (AIH)-like conditions post-COVID-19 vaccination, not observed during clinical trials. Liver injury has been observed with both vector- and messenger ribonucleic acid (mRNA)-based vaccines with a varying period of vaccination-to-symptom onset.
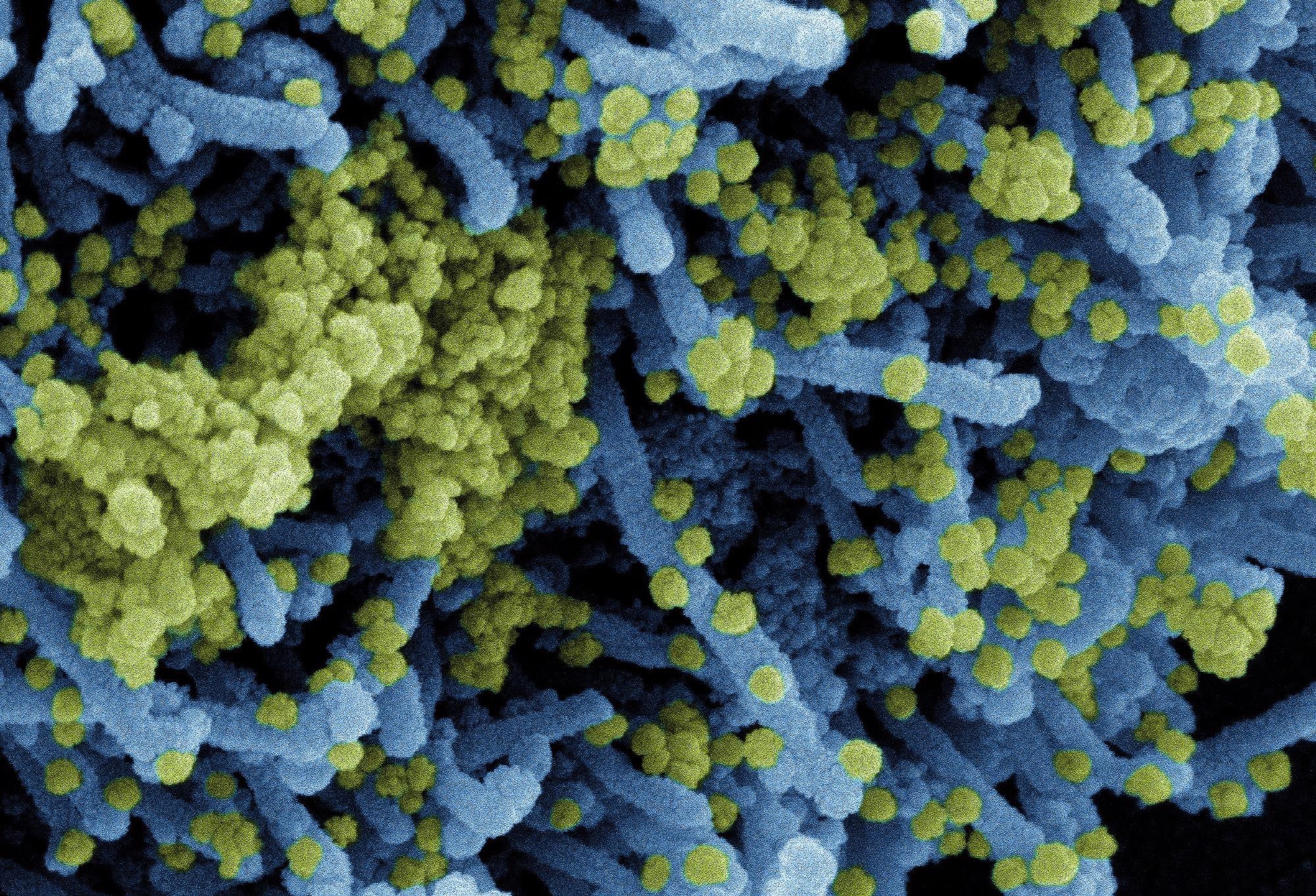 Study: SARS-CoV-2 vaccination can elicit a CD8 T-cell dominant hepatitis. Image Credit: NIAID
Study: SARS-CoV-2 vaccination can elicit a CD8 T-cell dominant hepatitis. Image Credit: NIAID
The study and findings
In the present study, researchers described the case of a male who presented with acute mixed hepatitis post-first BNT162b2 vaccine dose and severe hepatitis post-second dose.
The patient, aged 52 years, had no medical history except hypothyroidism and developed nausea, pruritus, loss of appetite, and fatigue. The onset of symptoms was about 10 days after the first BNT162b2 dose. Subsequently, the patient developed jaundice, and a liver function test (LFT) indicated acute mixed hepatocellular/cholestatic hepatitis and was admitted to a primary care center after 25 days of first vaccination.
Hepatitis A, B, C, or E virus, cytomegalovirus (CMV), and Epstein-Barr virus- infections were ruled out as the cause based on serological or polymerase chain reaction (PCR) tests. Forty-one days post-first dose, the patient took a second BNT162b2 vaccine, and 20 days after the second dose, the patient had fatigue and nausea. Laboratory testing confirmed the relapse of acute mixed hepatitis, and 26 days after the second vaccination, the case was referred to the tertiary care center.
Autoimmune serological tests revealed mild hyperglobulinemia, antinuclear antibodies (ANA), and borderline positivity for anti-mitochondrial M2 antibody (AMA-M2) and anti-smooth muscle antibodies, while anti-liver kidney microsomal (LKM) antibody tests were negative. The liver biopsy revealed interface hepatitis with moderate lymphoplasmacytic infiltrate and lobular necrotic and apoptotic foci. These clinical findings were consistent with a probable AIH, and the treatment was 9 mg of budesonide/day. In the ensuing weeks, levels of liver enzymes dropped, and another relapse occurred after 39 days of therapy initiation, controlled by systemic steroids and ursodeoxycholic acid. LFTs normalized in eight weeks, and anti-spike (S) antibodies showed no significant fluctuations.
Further, the team found infiltrates of T and B lymphocytes, macrophages, granulocytes, and plasma cells in the liver. A 5.3-fold increase in immune cells was observed relative to control (non-diseased) tissue. The cluster of differentiation 8 (CD8) T lymphocytes was the most abundant among immune cells, a condition unanticipated for AIH. Contrastingly, B and plasma cells were relatively lower, unlike typical AIH presentations, albeit more enriched than controls. Spatial analysis of liver parenchyma for different subsets of immune cells revealed more extensive immune infiltration in the periportal areas. While B and plasma cells were enriched predominantly in the periportal regions, a panlobular distribution was noted for CD8 T lymphocytes. Notably, cytotoxic CD8 T cells (characterized by granzyme B) were highly accumulated, while the levels of other granzyme B-expressing cells remained unchanged.
Next, flow cytometry analyzed intrahepatic and peripheral populations of CD8 T cells in depth. The intrahepatic CD8 T cell pool showed enrichment of markers for activation (CD38) and tissue residency (CD103, CD69, and C-X-C Motif Chemokine Receptor 6 [CXCR6]). CD8 T cells in peripheral blood also expressed CD38. Intriguingly, CD38 expression was markedly higher in the patient (75.9%) than in control (15.4%) matched for post-vaccination time without hepatitis development. A 3.4-fold enrichment of SARS-CoV-2 S-specific CD8 T lymphocytes was noted in the intrahepatic CD8 T cell population compared to peripheral blood.
Moreover, S-specific CD8 T lymphocytes were 10.2-fold more abundant in the peripheral blood than T lymphocytes specific for an Epstein-Barr virus-specific T cell control epitope. A stable frequency of S-specific CD8 T cells was noted in circulation, and the CD38 levels decreased with budesonide therapy. Nevertheless, CD38 expression on CD8 T cells specific for SARS-CoV-2 S protein and other cytotoxic markers were elevated when a relapse occurred during budesonide treatment but normalized after treatment with systemic immunosuppressants.
Conclusions
The researchers noted a slight increase in peripheral immunoglobulins and intrahepatic enrichment of plasma and B cells. Strikingly, cytotoxic CD8 T cells (CD38-expressing) were the most enriched to the extent that they were the most abundant immune cells in the liver.
These observations implicated T cells as the pathogenic cell type associated with the vaccination-related immune hepatitis as the novel AIH subtype. These findings indicated that vaccination with BNT162b2 might cause immune-mediated hepatitis by vaccine-elicited cellular immunity mechanisms.
Journal reference:
- SARS-CoV-2 vaccination can elicit a CD8 T-cell dominant hepatitis, Boettler T, Csernalabics B, Salié H, Luxenburger H, Wischer L, Alizei ES, Zoldan K, Krimmel L, Bronsert P, Schwabenland M, Prinz M, Mogler C, Neumann-Haefelin C, Thimme R, Hofmann M, Bengsch B, Journal of Hepatology (2022), DOI: https://doi.org/10.1016/j.jhep.2022.03.040, https://www.sciencedirect.com/science/article/pii/S0168827822002343