Globally, the Coronavirus Disease 2019 (COVID 19) pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has disrupted people's daily lives due to restrictions such as frequent lockdowns and social distancing guidelines. Children with neurodevelopmental disorders (NDDs) are especially vulnerable to emotional and behavioral changes during a pandemic.
The data for the analysis was derived from parents' responses to the Coronavirus Health and Impact Survey Initiative (CRISIS), which was adapted to assess Autism and Related Neurodevelopmental Conditions (AFAR). CRISIS predicted the risks among the general population by determining the perceived risks, worries, and life changes amidst the pandemic. It also considered the mental health pre and post COVID-19 pandemic. Investigators from across the globe collected the survey data for this study.
The purpose of the study was to quantify changes in aspects impacting the daily lives of patients with NDD/ASD, including therapeutic services. In addition, subgroups and predictors of impact were identified.
A cohort of 1,275 individuals was included – 1,004 individuals had ASD, 214 were patients of attention-deficit/hyperactivity disorder (ADHD) without ASD, and 57 individuals suffered from other types of NDD, but not ASD.
Intelligence estimates were available for 938 patients – 624 patients scored average or above average; 141 patients were borderline intelligent, and 173 patients suffering from varying degrees of intellectual disability.
While 64% of the caregivers had a college or higher degree, 30% had a high school degree, and 6% had elementary education. More than half of the literate population hailed from European/British ancestry.
The changing symptoms and access to therapeutic services during the early stages of the pandemic were assessed. Four ASD/NDD subgroups were identified with distinctive patterns of symptom or service changes – 53% with average changes in symptom or service; 23% with primarily modified services; 20% comprising only broad symptom worsening cases; and 6% with primarily lost services.
Prediction of COVID-19 Impact
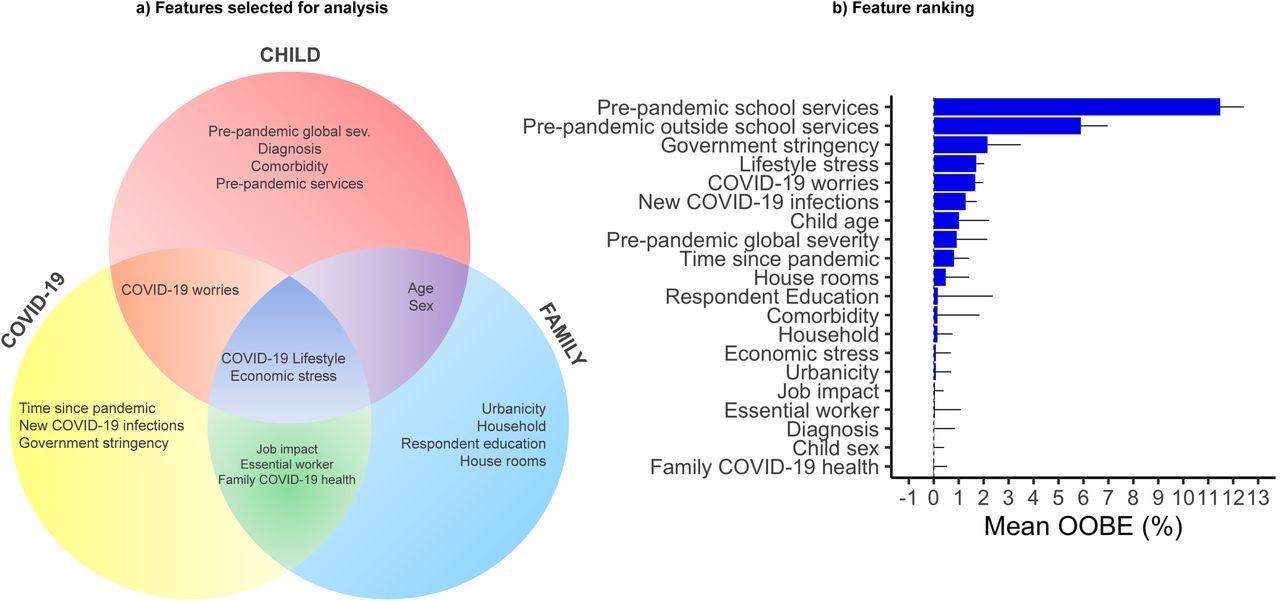
a) The Venn diagram shows the 20 features selected for the Random Forest analysis across three partially overlapping domains: Child (socio– demographics, clinical characteristics before and during the pandemic; in red); COVID-19 pandemic factors (COVID-19 rates and related restrictions, and time since pandemic started; in yellow); and Family/Household factors (urbanicity, household composition and respondent education; blue). b) Feature ranking by mean OOBE importance plot across the 20 features included in the Random Forest model shown in descendent order. Abbreviations: OOBE, average out-of-bag error.
Individuals with stable symptoms were divided into three subgroups, which helped identify the risk and protective factors. These symbolized the different pathways leading to stabilization or worsening of clinical situations.
Other predictors were found to be specific to ASD/NDD patients and age. The impact of the pandemic on young individuals with ASD/NDD was thereby a result of a combination of ASD/NDD specific and universal context related to service changes, pre-and post-pandemic.
The results revealed a significant worsening of sleeping problems from pre- to post-COVID 19. Of note, 20% of the cohort showed worsening symptoms that impacted their daily living skills, internalizing, externalizing symptoms, restricted and repetitive behaviors (RRB), and sleep. In addition, a number of disruptions in health services were encountered by patients, like switching to telemedicine or loss of services.
The difference in access to the services formed three subgroups among clinically stable patients based on symptom changes and clustering services, enabling the precise identification of the resilience and risk factors.
The most relevant predictors of the impact of the pandemic remained common risk factors that were comparable among the general population and those specific to ASD/NDD and age.
It was noted the importance of understanding how a crisis impacts different clinical groups. It was also found that older children experienced the least pandemic-associated changes.
The study revealed that maintaining even a modified form of therapeutic services during the COVID-19-associated restrictions can render a more clinically stable situation. This was evident through the observation that the subgroup with a vast range of lost services experienced greater impairment.
Conclusion
A concurrent assessment of both symptoms and service access is critical to understanding the heterogeneous impact of the pandemic on ASD/NDD youth. Using the data, it was possible to define pathways to risk and resilience that included both universal and ASD/NDD-specific contributors.
Overall, the COVID-19 pandemic impact on ASD/NDD youth varies as in the general population. During pre- and pandemic situations, service disruptions are contextualized by risk and resilience. In preparation for and during disasters, providing mental healthcare is critical for ASD/NDD youth - further motivating efforts to assess the effectiveness of telehealth and/or hybrid treatment programs. Additionally, this study highlights the importance of international data sharing and collaboration in addressing the needs of the most vulnerable.
Source:
- Vibert, B., Segura, P., Gallagher, L., et al. (2022). CRISIS AFAR: An International Collaborative Study of the Impact of the COVID-19 Pandemic on Youth with Autism and Neurodevelopmental Conditions. medRxiv* preprint. doi: 10.1101/2022.04.27.22274269. https://www.medrxiv.org/content/10.1101/2022.04.27.22274269v1