In a recent study under review in the Journal of Hematology & Oncology journal and currently available on the Research Square* preprint server, researchers investigated the presence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike protein (SP) in the thrombi (or blood clots). They retrieved the thrombi from coronavirus disease 2019 (COVID-19) patients with acute ischemic stroke (AIS) and acute myocardial infarction (AMI).
 Study: Evidence of SARS-CoV-2 Spike protein on retrieved thrombi from COVID-19 patients. Image Credit: Kateryna Kon / Shutterstock
Study: Evidence of SARS-CoV-2 Spike protein on retrieved thrombi from COVID-19 patients. Image Credit: Kateryna Kon / Shutterstock

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
COVID-19 patients commonly suffer from thrombotic complications. However, the pathophysiology of COVID-19-associated coagulopathy is complex and not fully elucidated. Studies have discovered free SP fragments in the plasma of COVID-19 patients. Although rare, SARS-CoV-2 has been found in the thrombi retrieved from brain arteries of AIS patients and more frequently in the coronary arteries of AMI patients.
Accordingly, the researchers tested the hypothesis that the SP activates the coagulation cascade by binding angiotensin-converting enzyme 2 (ACE2) directly on platelets and endothelial cells. Additionally, they investigated whether circulating SP induces hypercoagulability by directly interacting with fibrin or fibrinogen.
About the study
In the current study, researchers enrolled all the study participants post their admission to the emergency department (ED) of Policlinico Umberto I hospital, University of Rome La Sapienza, between March 2020 and April 2021.
They enrolled four COVID-19-positive patients, three with large vessel occlusion (LVO)-acute ischemic stroke (AIS) and one with acute myocardial infarct (AMI). The mean age of three LVO-AIS patients was 67 years, three were male, and one patient had received intravenous thrombolysis treatment. The fourth AMI patient was a 43-year-old male. On a pulmonary computed tomography (CT) scan, all the COVID-19-positive patients had lung ground-glass opacity.
The control group comprised four LVO-AIS patients without SARS-CoV-2 infection. The mean age of control group patients was 69 years, and three of the four patients had received intravenous thrombolysis.
The researchers retrieved each patient's thrombus by mechanical thrombectomy. Subsequently, they fixed thrombi in 10% formalin, stained their sections with hematoxylin and eosin (H&E), and embedded them in paraffin.
Further, the researchers performed double immunofluorescence to co-localize platelets with SARS-CoV-2 SP for visualization. They also extracted SARS-CoV-2 ribonucleic acid (RNA) from clots using an RNA kit and amplified RNA using a real-time reverse transcription-polymerase chain reaction (RT-PCR) system for qualitative RNA detection.
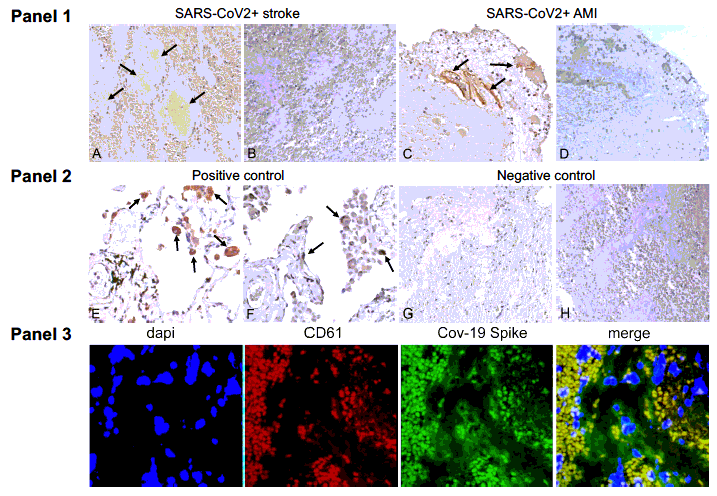
Arterial thrombi from Covid-19+ patients contain Sars-CoV-2 SP but not N protein Panel 1. Positive immunostaining for SARS-CoV-2 Spike protein (SP) (arrows) in representative thrombotic material from COVID19+ patients, retrieved from cerebral (A) and coronary (C) arteries. Immunohistochemistry for Nucleocapsid protein (NP) was negative in the same samples (B-D). Panel 2. Representative positive immunohistochemical staining for SP (E) and NP (F) (arrows) in the lung of a patient affected by COVID-19 (positive control). Representative negative immunostaining for SP (G) and NP (H) in a thrombus retrieved from the middle cerebral artery of a patient not affected by COVID-19 (negative control). Original magnification 20X. Panel 3. Double immunofluorescence of thrombotic material retrieved from COVID19+ patient cerebral artery. Platelets are stained with antibodies CD61 (red) and SARS-CoV-2 Spike Protein (SP) (green). Overlap of SARS-CoV-2 SP and platelets is shown in yellow (merge).
Results and conclusion
The test subjects and controls had similar amounts of platelets and red blood cells or fibrin. The COVID-19-positive thrombus retrieved from the anterior descending coronary artery showed substantial SP immunostaining, while COVID-19-positive thrombi retrieved from cerebral arteries showed mild positivity for SP. None of the thrombi had cells with NP.
The authors noted that most of the SP co-localized with platelets. On the other hand, RT-PCR could not detect SARS-CoV-2 RNA in all three COVID-19-positive thrombi.
According to the authors, one other study attempted to identify SP in retrieved thrombi from six AIS patients; however, they did not get any positive results. Contrastingly, the current study supported the hypothesis that free SP fragments, not the whole SARS-CoV-2, trigger the platelet activation and clot formation in COVID-19. One plausible explanation is that platelets and endothelial cells express genetically diverse ACE2 receptors. Another explanation could be the use of different kinds of polyclonal anti-SP antibodies used in the current study or the varying burden of COVID-19 on stroke pathogenesis.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Manuela De Michele, Giulia d'Amati, Martina Leopizzi, Marta Iacobucci, Irene Berto, Svetlana Lorenzano, Laura Mazzuti, Ombretta Turriziani, Oscar G. Schiavo, Danilo Toni, Evidence of SARS-CoV-2 Spike protein on retrieved thrombi from COVID-19 patients, Research Square pre-print 2022, DOI: https://doi.org/10.21203/rs.3.rs-1614096/v1, https://www.researchsquare.com/article/rs-1614096/v1
- Peer reviewed and published scientific report.
De Michele, Manuela, Giulia d’Amati, Martina Leopizzi, Marta Iacobucci, Irene Berto, Svetlana Lorenzano, Laura Mazzuti, Ombretta Turriziani, Oscar G. Schiavo, and Danilo Toni. 2022. “Evidence of SARS-CoV-2 Spike Protein on Retrieved Thrombi from COVID-19 Patients.” Journal of Hematology & Oncology 15 (1). https://doi.org/10.1186/s13045-022-01329-w. https://jhoonline.biomedcentral.com/articles/10.1186/s13045-022-01329-w.