Scientists have recently analyzed the association between herpesviruses and type 2 diabetes. This study is available in the journal Diabetologia.
Typically, humans are infected by eight different herpes viruses, namely, herpes simplex viruses (HSV), Epstein–Barr virus (EBV), varicella-zoster virus (VZV), cytomegalovirus (CMV), and human herpesviruses (HHV). All these viruses can cause lifelong latent infection after initial mild systemic infection.
Type 2 diabetes is one of the most common metabolic diseases. An individual is known to be prediabetic when diagnosed with impaired glucose tolerance (IGT) or impaired fasting glucose (IFG). Studies have shown that persons with prediabetes are significantly more likely to develop type 2 diabetes than those with normal glucose levels. In addition, several studies have identified both genetic factors as well as other relevant factors, such as obesity, unhealthy diet, and inflammation, which enhance the risks of type 2 diabetes.
Researchers have found that type 2 diabetes reduces the body's innate and adaptive immune capacities, thus making an individual more susceptible to infection. A high volume of research has shown that diabetes enhances the risk of viral infection. These studies have reported that individuals with diabetes are at a greater risk of contracting severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), hepatitis B, and hepatitis C infection.
Recently, scientists have established an aetiological connection between viruses, namely, enteroviruses and Coxsackie, and type 1 diabetes. Interestingly, an increased prevalence of HHV8 has been observed among type 2 diabetic patients in multiple populations. Further longitudinal studies are therefore needed to understand the potential link between herpesvirus infection and (pre)diabetes.
The Connection between Viruses and Diabetes - A New Study
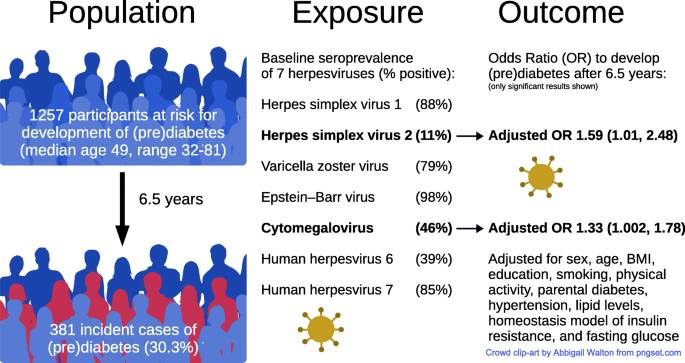
The present longitudinal population-based cohort study has investigated the association of the seven herpesviruses, i.e., HSV1, HSV2, VZV, EBV, CMV, HHV6, and HHV7, with the incidence of (pre)diabetes. In addition, researchers have cross-sectionally analyzed their relationship with HbA1c (average blood sugar measure for the last two months).
Scientists obtained data from KORA, a population-based health research platform in Germany. They conducted follow-up studies of the KORA study cohort using the F4 (2006–2008) and FF4 (2013–2014) studies. Researchers identified candidates with normal glucose tolerance at baseline. These candidates were at a higher risk of (pre)diabetes. All the participants underwent extensive phenotyping, including viral multiplex serology for human herpesviruses, oral glucose tolerance test (OGTT), and HbA1c.
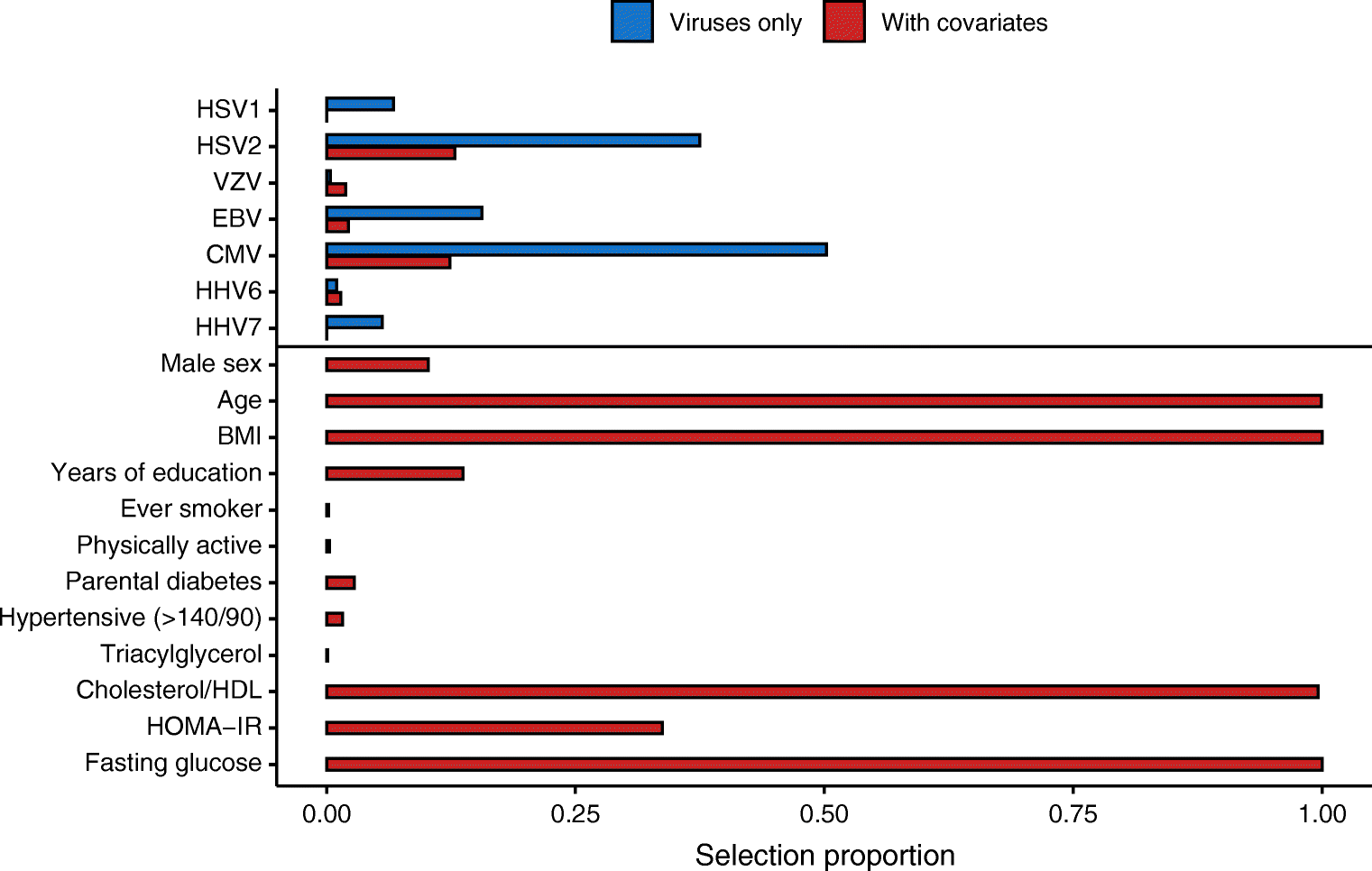 Selection proportion of viruses and confounders in two logistic LASSO models on (pre)diabetes incidence (n = 1257 participants). The first model (blue) only includes the serostatus for the seven assayed herpesviruses, and the second model (red) further includes confounders. We report the selection proportion calculated over 1000 calibrated models fitted on 80% of the full population, each including the same proportion of incident cases. For each model, the penalty was calibrated using fivefold cross-validation. The selection proportion of each variable was derived by summing the number of times it was included across the 1000 models β (95% CI)
Selection proportion of viruses and confounders in two logistic LASSO models on (pre)diabetes incidence (n = 1257 participants). The first model (blue) only includes the serostatus for the seven assayed herpesviruses, and the second model (red) further includes confounders. We report the selection proportion calculated over 1000 calibrated models fitted on 80% of the full population, each including the same proportion of incident cases. For each model, the penalty was calibrated using fivefold cross-validation. The selection proportion of each variable was derived by summing the number of times it was included across the 1000 models β (95% CI)
Key Findings
Researchers limited their studies to participants with normal glucose tolerance at baseline to reduce the risk of reverse causality. The current study reported a correlation between seropositivity for HSV2 and CMV, and (pre)diabetes incidence. Multivariate analysis revealed that the above-mentioned viruses consistently influence the prevalence of (pre)diabetes, independent of education, age, smoking, sex, BMI, physical activity, hypertension, insulin resistance, lipid levels, and fasting glucose.
Scientists observed that HSV2 was cross-sectionally linked with HbA1c, independently of the confounders mentioned above. Even though it is unlikely that marginal enhancement in blood glucose levels in non-diabetic individuals would compromise the immune system, cross-sectional modeling failed to distinguish between causal effect directions.
Although previous studies stated that herpesviruses are persistent in the host, they might not be detected via antibody analysis in the blood due to the changes in the host immune system or viral activity. Scientists stated that in most cases infection due to herpesvirus occurs in early childhood; however, infection at later ages is possible. Hence, the seroconversion observed in this study indicates the incident cases, which might be because of an increased antibody reactivity of a previously undetectable virus. Researchers stated that an individual without seropositivity does not mean that he/she is healed because the virus might be in its undetectable latency state.
Limitation of this Current Study
One of the limitations of the current study is that the serological analysis did not capture the past infections fully. Typically, the level of antibodies is influenced by the severity of the infection, the strength of immune responses upon primary infection, virus-host interaction, and the potential of recurrent infections. In this study, researchers observed inconsistency in serostatus between two time points, which were not explained by incident cases.
Scientists lacked relevant information related to acute herpesvirus manifestations from the study cohort, which is why they were unable to determine the underlying cause behind the observed seroconversion. Another limitation of the study is that the viral multiplex assay for HHV6 and HHV7 was not validated. This is because of the lack of availability of standardized multiplex assay.
Conclusion
The current study has established a link between HSV2 and CMV seropositivity with the incidence of (pre)diabetes after adjusting for confounding factors. It has also documented a cross-sectional association of HSV2 serostatus with HbA1c, independent of confounding factors. In the future, the pathomechanisms associated with HSV2 and CMV in (pre)diabetes development must be studied.