The ability of public health authorities to track disease incidence and transmission patterns has become a vital part of public health response and preparedness during the COVID-19 pandemic. Policymakers globally have applied staged regional mitigation frameworks, where the advancement of a region from one phase of mitigation policy to the next depends on certain indicators exceeding a specific threshold or comparative growth rate. However, typical public health metrics for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) surveillance might be skewed or fall behind shifting COVID-19 community transmission trends.
Sentinel populations, which have previously been used or suggested for monitoring pandemic and seasonal influenza, can be used to detect changes in COVID-19 transmission in the general population. SARS-CoV-2 monitoring on the sentinel community should be less susceptible to selection bias versus at-large diagnostic testing in the general population until testing parameters and sampling initiatives on the sentinel population remain established and do not vary over time.
About the study
The present study aimed to determine the patterns of COVID-19 transmission with minimal lag and bias in the United States (US) city of Chicago. For this, the team used details from individuals tested at the community-based testing services run by the Illinois Department of Public Health (IDPH) and the Chicago Department of Public Health (CDPH). Of note, these testing centers were established to enhance access of underrepresented populations for SARS-CoV-2 testing.
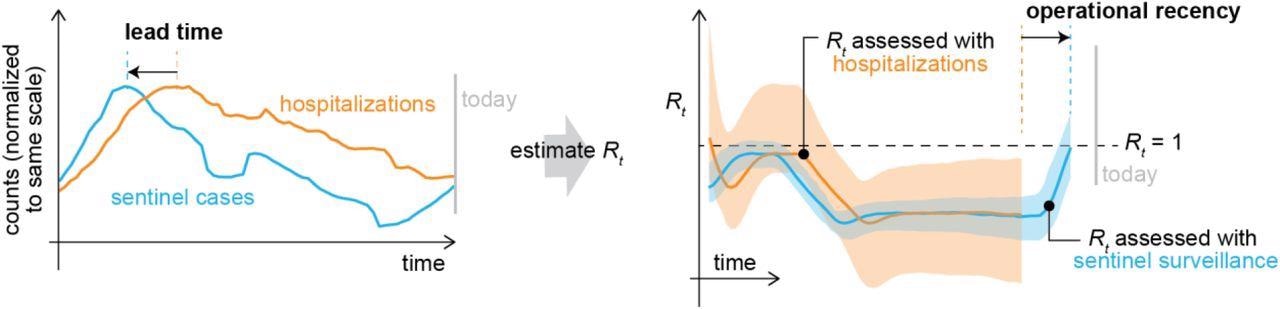
Theoretical diagram of the instantaneous effective reproductive number R(t) derived from hospitalizations (orange) and sentinel surveillance (blue). Because symptom onset typically occurs sooner in the course of disease than a visit to the emergency department or hospitalization, sentinel cases can return more recent estimates of R(t) than hospital-based indicators. With sufficient sample size, sentinel surveillance could also return more precise estimates of R(t).
Moreover, the authors reused the dataset to assess whether sentinel monitoring of newly symptomatic persons getting outpatient SARS-CoV-2 diagnostic testing could properly quantify the instantaneous reproductive number R(t), a community transmission measure, and offer early warning of COVID-19 transmission alterations. The sentinel group consisted of individuals tested at community-based COVID-19 diagnostic testing locations in Chicago from September 2020 to June 2021 and reported the onset of SARS-CoV-2 infection symptoms within four days of their test. The degree to which sentinel surveillance catches gold-standard admission patterns was examined. Besides, the team determined the operational recency and lead time of sentinel monitoring versus hospitalization data.
The researchers stated that since symptom initiation happens sooner after COVID-19 than hospitalization, the SARS-CoV-2 outpatient-based sentinel surveillance technique should provide operational recency above hospital-based metrics, enabling R(t) to be computed for more latest dates. Moreover, sentinel monitoring would offer data on transmission patterns in younger groups than the hospitalized cohort. Therefore, if transmission shifts arise first in younger individuals, it will lead to changes in sentinel surveillance data and ultimately contribute to alterations in hospitalizations.
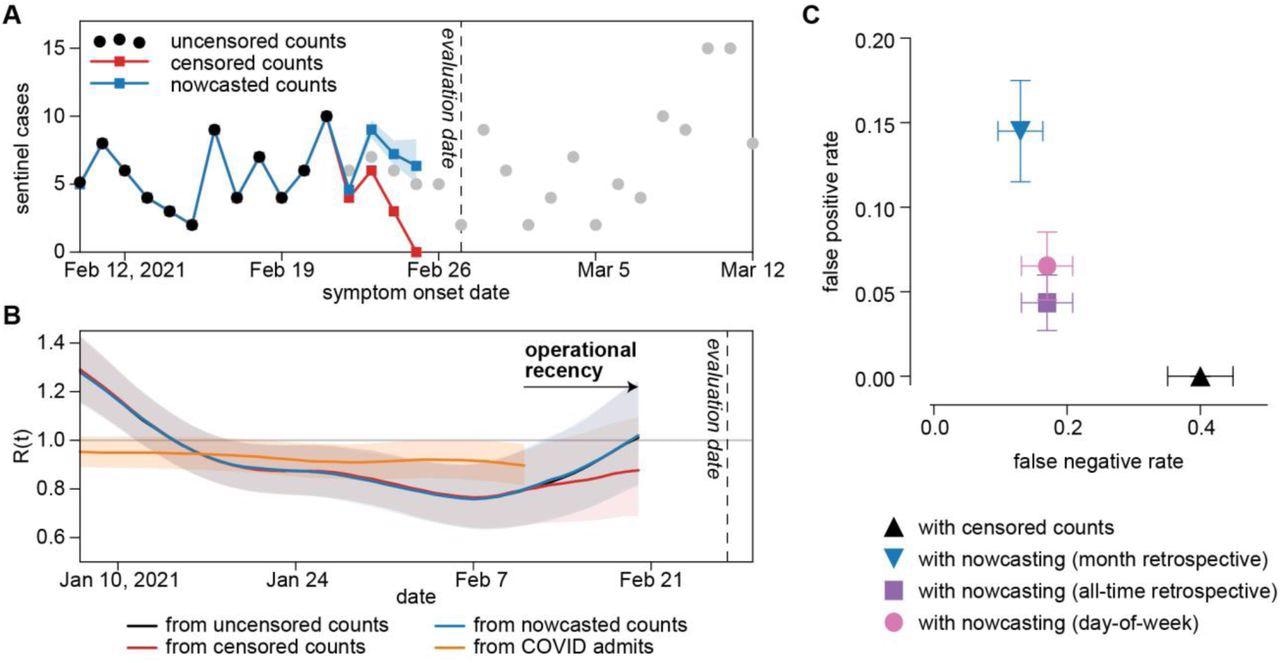
Operational performance of sentinel surveillance. A) Sentinel case counts for a representative evaluation date of February 27, 2021. Black dots: sentinel case counts fully accessible on the evaluation date. Gray dots: sentinel case counts partially accessible or not yet accessible on the evaluation date. Red dots: right-censored sentinel case counts available on the evaluation date. Blue dots: nowcasts sentinel case counts with a past-month retrospective model. Blue shaded region: 95% confidence interval for nowcasted counts. B) R(t) derived from uncensored sentinel cases, right-censored sentinel cases, nowcasted sentinel cases, and COVID-confirmed admissions for an evaluation date of February 27, 2021. C) False negative and false positive rates of R(t) derived from right-censored and nowcasted sentinel cases when compared to R(t) derived from uncensored case counts.
Results
The study results showed that the daily volume of sentinel samples varied significantly with time and the sentinel cohort was not demographic representatives of the Chicago population. However, R(t) approximated from sentinel cases was in fair accordance with R(t) projected from the hospital dataset in the general population. In Illinois, the SARS-CoV-2 pandemic did not impact the various ethnic and racial groups to the same degree, and the sentinel cohort was more Latino/Hispanic than the overall population. As a result, the minor variation between hospital-based and sentinel R(t) might imply the actual differences in COVID-19 transmission dynamics between the general and sentinel populations. However, considering the skewed sample frame of the sentinel cases, the overall agreement in hospital admissions R(t) and sentinel R(t) was noteworthy.
The naïve estimate for a retrospective lead time of changes in sentinel cases versus changes in hospitalizations was five to six days since symptoms were predicted to emerge an average of 5.5 days following infection and hospital admission happens an average of 11.1 days post-infection. The retrospective cross-correlation assessment indicated no noticeable lead time among sentinel cases and hospital-based metrics.
COVID-like illness emergency department visits (CLI ED), COVID-19-confirmed hospital admissions (COVID admits), CLI hospital admissions (CLI admits), and COVID-19-confirmed emergency department visits (COVID ED) had the best agreement between R(t) estimates. On 85.5% of dates, R(t) from sentinel cases matched to R(t) from COVID admissions.
Upon deployment in Chicago, the operational recency benefit of sentinel surveillance was evident. Entire data from sentinel testing was generally available after approximately two days, whereas those from hospital admissions took around five days. On a regular assessment date, the latest R(t) estimates from hospital admissions were for the previous 16 days, while those from sentinel monitoring were for the preceding seven days. Overall, there was a nine-day operational recency benefit for sentinel surveillance versus hospital admissions.
Conclusions
To summarize, the study findings illustrated that R(t) of COVID-19 obtained from sentinel cases matched well with R(t) calculated from other indicators in the US. There was no noticeable lead time between patterns in sentinel cases and COVID-19-linked hospitalizations retrospectively. Furthermore, sentinel monitoring had a nine-day operational recency benefit over hospital admissions during deployment. The positive results of opportunistic sentinel monitoring imply that well-structured COVID-19 outpatient sentinel tracking might give reliable early warning of rising SARS-CoV-2 transmission levels.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Tracking changes in SARS-CoV-2 transmission with a novel outpatient sentinel surveillance system in Chicago, USA; Reese Anthony Keith Richardson, Emile Jorgensen, Philip Arevalo, Tobias M Holden, Katelyn Gostic, Massimo Pacilli, Isaac Ghinai, Shannon Lightner, Sarah Cobey, Jaline Gerardin. medRxiv preprint 2022, DOI: https://doi.org/10.1101/2022.05.10.22274869, https://www.medrxiv.org/content/10.1101/2022.05.10.22274869v1
- Peer reviewed and published scientific report.
Richardson, Reese, Emile Jorgensen, Philip Arevalo, Tobias M. Holden, Katelyn M. Gostic, Massimo Pacilli, Isaac Ghinai, Shannon Lightner, Sarah Cobey, and Jaline Gerardin. 2022. “Tracking Changes in SARS-CoV-2 Transmission with a Novel Outpatient Sentinel Surveillance System in Chicago, USA.” Nature Communications 13 (1): 5547. https://doi.org/10.1038/s41467-022-33317-6, https://www.nature.com/articles/s41467-022-33317-6.