Emerging adulthood is a critical period for neuronal development, neuroplasticity, and maturation of the hypothalamic-pituitary–adrenal axis. During this period, stress responses, including fluctuation in hormonal levels and diverse activation of the hypothalamic-pituitary-adrenal axis, significantly impact the development of mental health. Studies have shown that mental illnesses frequently occur in emerging adults during this period.
The gut microbiota is a collection of diverse microorganisms, including bacteria, residing in the gastrointestinal tract. Various factors, including genetic factors, early-life factors (maternal infection, antibiotic use, etc.), and environmental/lifestyle factors (diet, physical activity, stress, etc.), can severely alter the composition and diversity of gut microbiota.
Recent evidence indicates that emerging adulthood is associated with a unique vulnerability in the gut microbiota. In emerging adults, the gut microbiota is less diverse, simple, and more unstable than in children, adolescents, and older people. In the current article, the scientists have hypothesized that the gut-brain-microbiota axis might play a role in determining mental health issues, which are significantly increasing in western countries, most probably because of unfavorable lifestyle behaviors.
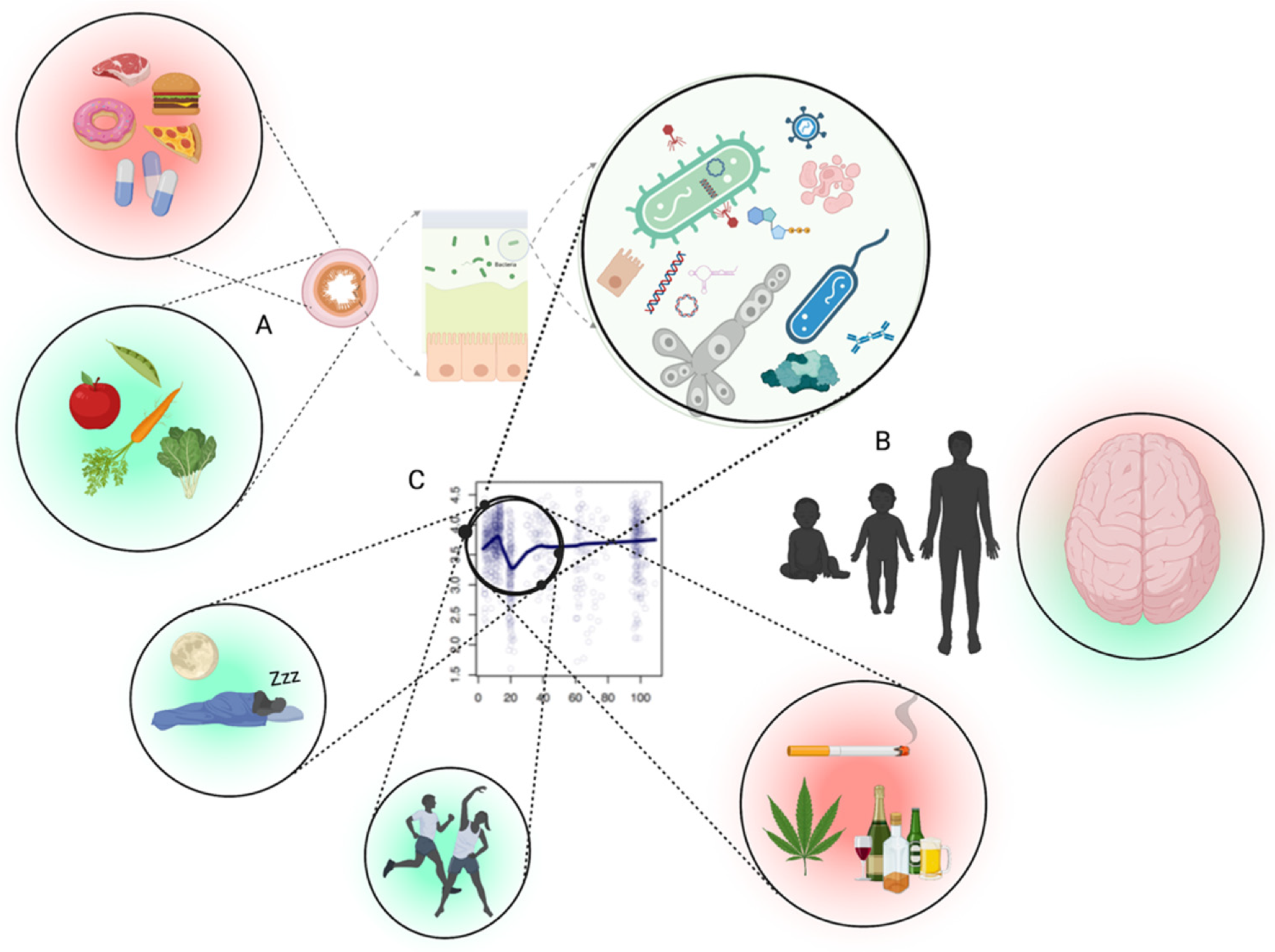 Interface between the gut microbiota and mental health likely depends upon several factors. (A) The first being the inputs to the intestinal tract which shape the microbiota accordingly (diet, medication, antimicrobials, etc.). (B) Periods where microbiota goes through changes in diversity (alpha) occur in healthy people, especially between late teens and early twenties, which likely result in differences of metabolic output which impact brain health. (C) The intersection of the adolescent brain, combined with a normally fluctuating microbiota of the age group, the promotion of a desirable microbiota through physical activity/exercise and circadian rhythm, and less desirable microbiota using different substances. Part (C) adapted from Bian et al., 2017. Figure created with Biorender (accessed on 29 April 2022).
Interface between the gut microbiota and mental health likely depends upon several factors. (A) The first being the inputs to the intestinal tract which shape the microbiota accordingly (diet, medication, antimicrobials, etc.). (B) Periods where microbiota goes through changes in diversity (alpha) occur in healthy people, especially between late teens and early twenties, which likely result in differences of metabolic output which impact brain health. (C) The intersection of the adolescent brain, combined with a normally fluctuating microbiota of the age group, the promotion of a desirable microbiota through physical activity/exercise and circadian rhythm, and less desirable microbiota using different substances. Part (C) adapted from Bian et al., 2017. Figure created with Biorender (accessed on 29 April 2022).
The gut-brain-microbiota axis
Microorganisms residing in the gut produce several vital components, such as short-chain fatty acids, brain-derived neurotrophic factors, and neurotransmitters, which mediate the communication between the gut and brain. An imbalance in gut microbiota can lead to microbial lipopolysaccharide (LPS)-mediated production of inflammatory cytokines, which subsequently affect the hypothalamic-pituitary–adrenal axis by stimulating the afferent vagal nerve.
Impact of gut microbiota on mental health
According to available literature, there is a link between gut microbiota and mental health. In this context, studies have shown that antibiotics-induced alteration in the gut microbiota is associated with altered emotional behaviors. The gut-brain-microbiota axis is known to play an essential role in the development of various neurological and psychiatric diseases, including Alzheimer’s disease, Parkinson’s disease, and autism spectrum disorder. Any imbalance in the gut microbiota during the period of emerging adulthood can induce a cascade of events that have prolonged negative impacts on both physical and mental health.
Impact of environment/lifestyle factors on gut microbiota and mental health
Environmental factors that have the highest impact on shaping the gut microbiota include diet, medications, and antimicrobial agents. In addition, physical activity, sleep patterns, and substance use considerably influence the gut microbiota as well as mental health.
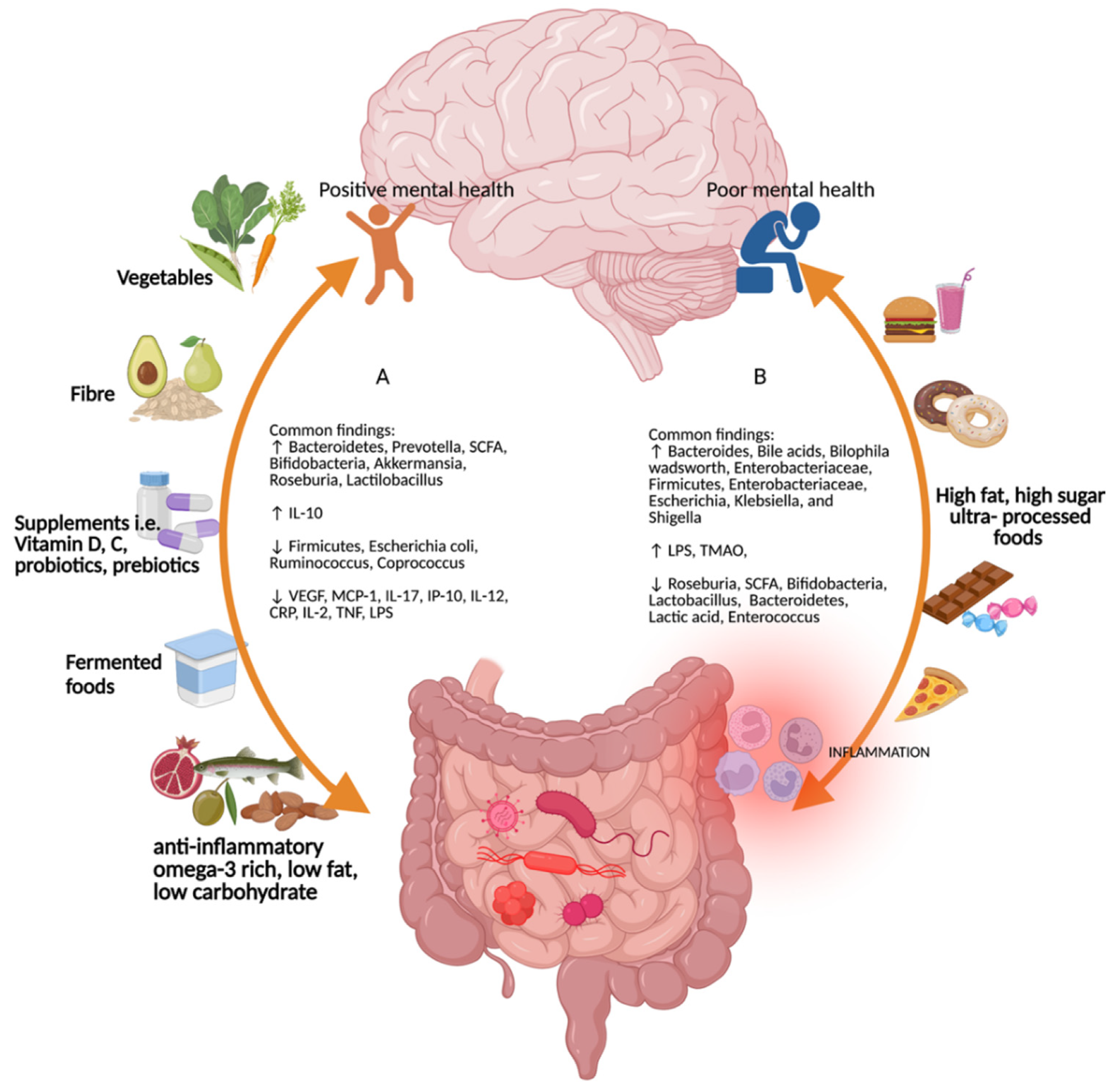 Common findings for the different types of diet on the gut–brain–microbiome axis. (A) Diets rich in vegetables, fiber, micronutrients such as vitamins D and C, probiotics and prebiotics, fermented foods, anti-inflammatory omega-3-rich, low-fat, and low-carbohydrate foods promote positive mental health and increases in Bacteroidetes, Prevotella, short-chain fatty acids, Bifodobacteria, Akkermansia, Roseburia, Lactilobacillus, and interleukin (IL)-10, and decreases in Firmicutes, Escherichia coli, Ruminococcus, Coprococcus, vascular endothelial growth factor, monocyte chemoattractant protein-1, interferon gamma-induced protein 10, IL-17, IL-12, c-reactive protein, IL-2, tumor necrosis factor, and lipopolysaccharide. (B) High-fat, high-sugar, and ultra-processed foods increase Bacteroides, bile acids, Bilophila wadsworth, Enterobacteriaceae, Firmicutes, Enterobacteriaceae, Escherichia, Klebsiella, and Shigella. Figure created with Biorender (accessed on 29 April 2022).
Common findings for the different types of diet on the gut–brain–microbiome axis. (A) Diets rich in vegetables, fiber, micronutrients such as vitamins D and C, probiotics and prebiotics, fermented foods, anti-inflammatory omega-3-rich, low-fat, and low-carbohydrate foods promote positive mental health and increases in Bacteroidetes, Prevotella, short-chain fatty acids, Bifodobacteria, Akkermansia, Roseburia, Lactilobacillus, and interleukin (IL)-10, and decreases in Firmicutes, Escherichia coli, Ruminococcus, Coprococcus, vascular endothelial growth factor, monocyte chemoattractant protein-1, interferon gamma-induced protein 10, IL-17, IL-12, c-reactive protein, IL-2, tumor necrosis factor, and lipopolysaccharide. (B) High-fat, high-sugar, and ultra-processed foods increase Bacteroides, bile acids, Bilophila wadsworth, Enterobacteriaceae, Firmicutes, Enterobacteriaceae, Escherichia, Klebsiella, and Shigella. Figure created with Biorender (accessed on 29 April 2022).
Diet
Dietary components significantly impact the composition and diversity of gut microbiota. Excessive consumption of unhealthy foods (saturated fat, refined sugar, red meat, and low-fiber foods) and lower consumption of healthy foods (fruits and vegetables) can induce microbial dysbiosis, which is characterized by alteration in functional composition, diversity, local distribution, and metabolic activities of gut microbiota.
Strong evidence indicates that a diet rich in vegetables, fruits, fibers, fermented foods, vitamins, probiotics, and polyunsaturated fatty acids helps maintain gut microbiota homeostasis and promotes positive mental health. In contrast, high-fat, high-carbohydrate, and ultra-processed foods are associated with gut dysbiosis, inflammation, and poor mental health.
Physical activity
It is well-known that regular physical activity is vital for maintaining metabolic and cardiovascular fitness and improving mental health. In addition, regarding gut microbial diversity, physical activity is known to increase the levels of beneficial microbes and metabolites in the gut.
The impact of physical activity may vary between individuals depending on the age, sex, genetic makeup, body mass index (BMI), and dietary habits. Notably, intense physical activity can induce gut microbiota dysbiosis and inflammation and cause adverse health consequences. Thus, the optimal level of physical activity needs to be individualized.
Substance use
Excessive consumption of nicotine, alcohol, cannabis and illegal substances has frequently been observed in emerging adults, especially those residing in Western countries. These substances are known to have a negative impact on both physical and mental health.
Neuronal nicotinic acetylcholine receptors are vital for the development and maturation of the central nervous system. Consumption of nicotine in early life can lead to addiction, cognitive decline, and psychiatric disorders. Moreover, nicotine consumption may induce gut microbiota imbalance by increasing the permeability of the intestinal mucosa and disrupting mucosal immune responses.
Excessive consumption of alcohol in early life can induce changes in the frontal and temporal brain lobes and disrupt the neural networks associated with learning, memory, psychomotor speed, attention, executive functioning, and impulsivity. In the gut, alcohol alters metabolite levels, increases inflammation, and disrupts intestinal epithelial integrity.
Cannabis consumption increases the activity of cannabinoid receptors and induces various health outcomes, including induction of gastric acid secretion, reduction of intestinal motility, and induction of intestinal permeability and inflammation. Moreover, studies have shown that early-life use of cannabis is associated with a decline in cognitive abilities.
Sleep pattern
Regular sleep patterns can be influenced by certain factors, including shift work, night-time light exposure, inconsistent timing of food intake, unhealthy eating, and jet lag. A shift in sleep timing and pattern is commonly observed among adolescents, associated with mental disorders such as depression and anxiety.
A disruption in sleep patterns can also disrupt the gut microbiome homeostasis by increasing harmful microbes and reducing beneficial microbes and metabolites.
Journal reference:
- Lee JE. 2022. Drugs, Guts, Brains, but Not Rock and Roll: The Need to Consider the Role of Gut Microbiota in Contemporary Mental Health and Wellness of Emerging Adults. International Journal of Molecular Sciences. https://www.mdpi.com/1422-0067/23/12/6643