Our mandate is to provide an integrated science-driven, peer-to-peer service to biotech and pharma companies that span both the preclinical and clinical phases of drug development. Our core expertise is in understanding immune system-mediated diseases and therapeutic modulation of the immune system.
Services include genetic, molecular, protein, cell and tissue analysis, cell and gene therapy bioanalytics, biomarker discovery, PK/PD, de novo assay method development, and validation. Our proprietary human in vivo translational research platform, ProtoTrials®, focuses on providing valuable early clinical insights and bridging the gap between preclinical and clinical phases.
What types of alternative multi-parameter flow cytometry approaches has Synexa developed?
Flow cytometry has long been used for routine assays, such as immunophenotyping, receptor occupancy, and to assess intracellular cytokine production. This is partly due to its versatility and the depth and volume of data that a single assay can produce.
However, as the technology and our understanding of the immune system have improved, the routine use of flow cytometry has expanded beyond these traditional uses. These include the analysis of antibody-dependent cellular cytotoxicity (ADCC), polyamine transport, anti-drug antibody (ADA) testing, cell-based PK assessment and phenotyping of extracellular vesicles. Immunomodulation has become an important therapeutic area for the treatment of a variety of diseases. This involves employing therapeutic monoclonal antibodies to treat diseases by activating immune-mediated responses.
Image Credit: tikisada/Shutterstock
What relevance do these approaches have when examining immune-mediated responses?
These responses are particularly pertinent in cancer and infectious diseases where antibodies can be utilized to induce an immune response against specific target cells. The mechanisms available for the induction of these responses include antibody-dependent cellular cytotoxicity, and these assays can target cell toxicity by the activation of host effector immune cells.
Measurement of the ADCC in vitro is commonly performed using chromium 51 release assays. However, whilst this assay is considered the gold standard to measure ADCC, it has many drawbacks, most significantly because it measures the release of chromium 51, which is a radioactive element, that is both dangerous and difficult to dispose of safely. Other assay formats that are commonly used to measure ADCC include colorimetric release assays, measuring lactate, dehydrogenase, or calcein release.
What challenges do you face when conducting ADCC assays using flow cytometry?
These assays often have a high level of background signal. Therefore, very little information is generated regarding the target or effector cell populations. At Synexa, we have developed a calcein AM retention assay as an alternative to these assay formats.
This novel assay format follows a similar concept to calcein AM release assays. However, instead of measuring the release of calcein AM into the culture supernatant, the labeled target cells are analyzed using a flow cytometer to measure calcein retention as a marker of live target cells. This assay is an attractive alternative to traditional assays because it provides more information on the co-culture environment and the cultured cells themselves. Less background signal is anticipated because each cell is visualized individually. This model is also advantageous because it can correct for nonspecific cell death with the inclusion of appropriate controls.
Could you describe how this worked in a case study?
During one study, Trastuzumab (Herceptin) was used as a therapeutic antibody in the flow cytometry assay. This antibody targets the HER2 receptor, which is overexpressed on breast cancer cells and is known to induce ADCC in cancer cell lines. In this study, we targeted cancer cells that were labeled with calcein AM, a non-fluorescent cell-permeable dye which is cleaved intracellularly in the cytoplasm.
Once cleaved, it releases a fluorescent signal that can be detected by the flow cytometer. These labeled cells retain the green fluorescence in their cytoplasm. However, when the cells die, this fluorescent molecule is released into the culture supernatant and is no longer detectable by the flow cytometer.
What is involved in the ADCC assay process?
ADCC is often mediated by natural killer cells or cytotoxic T cells. However, monocytes, macrophages, and granulocytes can play a role in inducing ADCC. Both NK cells and cytotoxic T cells induce cell death by releasing cytolytic molecules. Such a release is stimulated by the binding of the therapeutic antibody to the Fc gamma receptor on effector cells.
Fc-receptor binding occurs after the therapeutic antibody has undergone conformational changes induced by binding of the antibody to its cognate antigen on the target cell. Upon co-culture of target cancer cells with the therapeutic antibody in the presence of appropriate effector cells in the correct ration, target cell death can be monitored by calculating the number of calcein AM-positive cells in antibody-treated samples relative to the number of calcein AM-positive cells in the control sample, which in this case would be the non-treated sample.
Image Credit: Design_Cells/Shutterstock
How do you decide on what controls should be selected for use in these assays?
Appropriate gating and assay controls are critical for assay performance and accurate determination of ADCC. These include unstained target cells, calcein AM-stained target cells in the absence of antibody and effector cells, effector cells alone, as well as an appropriate negative control, which in this case would be no therapeutic antibody for each of the conditions that are assayed.
Additional viability dyes may also be included in this assay format to measure both live and dead cells in culture simultaneously. Overall, the data from these experiments represent an example of how this format can be applied for the assessment of ADCC, which is feasible, dynamic, and a functional alternative to the transitional calcein or chromium release assays.
What are the added benefits of using flow cytometry for ADA safety testing?
ADA generated against a pharmaceutical may be harmless or could lead to an unwanted immune response that could reduce the therapeutic effect of the pharmaceutical product, alter the pharmacokinetics or affect the clearance rate of the pharmaceutical. It is therefore important to assess and characterize ADAs when considering the safety of a pharmaceutical.
The current gold standard for ADA testing most often relies on immunoassays, such as ELISA. Whilst ADA and immunoassays generally have a high level of specificity for the detection of ADAs, a proportion of ADAs do not elicit a functional immune response or influence the pharmacokinetics of the drug. Therefore, these assays can have a high false positivity rate. The application of functional flow cytometry assays in conjunction with traditional ADA assays to determine the immunogenicity and functionality of ADAs is thus becoming more widely utilized.
Are functional ADA assays beneficial for the preclinical phase of drug development?
Yes, however, when developing and validating functional flow cytometry assays for ADA testing, various factors should be considered to develop an assay that has both high sensitivity and specificity. Some of these factors include the selection of the optimal sample matrix, screening for appropriate healthy donors where that is relevant, determining robust positivity criteria, and including appropriate assay controls.
Where possible, various sample matrices should be tested. The use of an inappropriate sample matrix, for example, serum instead of plasma, can lead to high levels of assay background and result in the inaccurate interpretation of data. Where samples from healthy volunteers are required for the assay, screening of the appropriate donors is essential.
The robustness of an assay’s positivity criteria increases as a greater number of samples are tested, ensuring that the assay has both high specificity and sensitivity. The assay should investigate and include appropriate controls to ensure accurate results. When the appropriate assay conditions are considered, this assay can successfully be used as a confirmatory assay for positive ADA results generated using an immunoassay.
How can flow cytometry be used to assess pharmacokinetics of a therapeutic agent?
Drug advancement and the direction it is moving in has paved the way for cell-based PK analysis, while tailor-made assay design allows for specific targeting of the drug or biomarker of interest, including small and large molecules and specific cell subsets.
The advantages of cell-based PK assessments include the potential for sampling from a variety of different matrices, the potential to target intracellular and surface markers, either individually or together, and the ability to perform real-time analysis or batched analysis, depending on the matrix and the specific assay validation parameters. Cell-based PK assays using flow cytometry can be developed and validated with a high degree of sensitivity and robustness to allow for implementation in clinical trials as an alternative to traditional ligand-binding assays.
Are there any other key areas of focus you are excited about at Synexa?
We are particularly interested in extracellular vesicles (EVs). EVs are excreted from several cell types and function to transport a variety of biomolecules, including nucleic acids, mRNA, proteins, lipids, and different metabolites between cells, and are thought to form part of the intracellular communication network.
To date, research has focused on the ability of EVs to modulate the immune system, both in normal and pathological processes. EVs are heterogeneous in nature and can be classified into two broad types, exosomes and ectosomes, which include microparticles.
What are the differences between exosomes and ectosomes, and what relevance do they have in drug development?
Ectosomes are formed by budding outwardly from the surface of the cell membrane and range in size from approximately a hundred to a thousand nanometers in diameter, while exosomes are produced by endocytosis and the formation of multivesicular bodies, which later fuse with the plasma membrane for excretion.
The primary difference between exosomes and ectosomes is their size, with exosomes being smaller, between 30 and 150 nanometers in diameter. As EVs have been associated with the ability to alter the biological response of the accepting cell, their applications are broad, ranging from diagnostic tools, therapeutic agents, or possible drug delivery vectors. While these applications are proposed, the majority of the initial research performed on EVs centers around their isolation, classification and function.
What methods are Synexa developing to analyze EVs in a clinical setting?
Synexa has been investing in developing methods to accurately quantify and characterize EVs, which are technically challenging due to their heterogeneity and size. Several approaches and technologies exist for this purpose. However, none of these approaches have demonstrated the ability to determine the full range of EV properties such as size, distribution, and biochemical composition.
Common methods used include microscopy, both electron and anatomic force microscopy, nanoparticle tracking analysis, or NTA and flow cytometry. These methods are often used in combination. Nanoflow cytometry also offers the ability to detect and quantify EV subpopulations from a variety of different origins down to the individual level, making it one of the technologies commonly employed for EV detection and phenotyping.
Could you explain how Nanoflow cytometry can be used for EV analysis?
Considerable challenges arise in the isolation and purification of EVs, adding to the complexity of assay development. These can be divided into pre-analytical and analytical considerations. Pre-analytical considerations include the source of the sample, sample collection, sample storage and sample size.
Once collected, the sample’s manipulation from isolation, purification, and storage can greatly influence EV recovery. Isolation or purification of EVs resulting in high concentration and purity of the sample is paramount for their study. Flow cytometry uses the principle of light scatter due to differences in refractive indices, and fluorescent detection. Nanoflow cytometers have enabled the detection and characterization of EVs due to a reduction in electronic noise and increased fluorescent detection, allowing for the characterization of individual EVs.
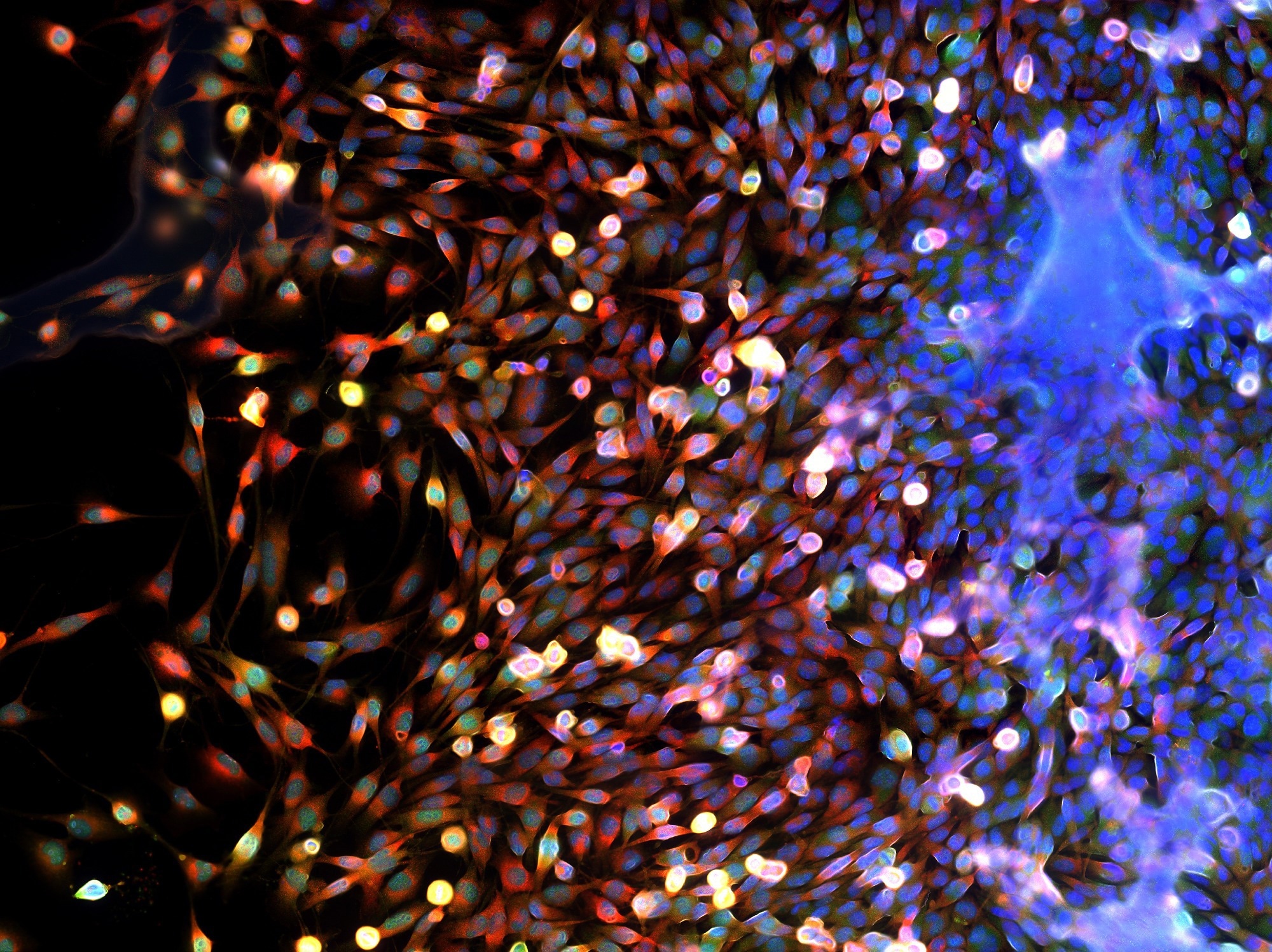
Image Credit: Damian Ryszawy/Shutterstock
What are the key scientific considerations and technical questions we should ask when developing a flow cytometry protocol?
The first consideration should always be that the protocol is fit for purpose. It really depends on the analyte that needs to be assessed as well as the sample matrix that will be used to detect the analytes. I also think that for flow cytometry assays specifically, or any cell-based assays, particular attention should be paid to matrix stability. These considerations need to be built in as part of the method development process to assess different stabilizing methodologies, if required, or else to assess the stability of the raw sample before processing and acquisition. Similarly, the validation approach for assays that will be taken into the clinical phase needs to be fit for purpose and ensure that the assay is sensitive and robust enough for its intended use.
During method development, what's the most important factor a sponsor should consider?
There are many mistakes that are made when developing assays and the most common is not necessarily considering the ultimate purpose of the assay; in what context is planned to be used, is this an assay that is being developed for preclinical assessment, or is it going to be used in the clinical setting? With that in mind, considerations need to be made about appropriate reagents that can be used as controls when developing assays; the sample matrix that will be used is also very important. I think a big mistake is not considering the end game for an assay and planning for how it will ultimately be used.
How can these insightful flow-based assays complement other platforms in a clinical study?
A good example of this is the ADA assay format looking at functional responses to anti-drug antibodies. In this context, for example, the functional assay is used in combination with the traditional ADA immunoassay format to detect ADAs. It offers users a depth of information regarding the functionality of these antibodies and the ultimate effect or outcome for the patient in which these antibodies are detected. Flow cytometry and any cell-based assays have the ability to offer a wealth of data if they are designed and implemented correctly. There are definite instances where flow cytometry and these types of methodologies can be applied in the clinical phase alongside other more traditional assay formats.
About Natalie Strickland
Natalie Strickland, Global Head of Translational Science at Synexa. Natalie received her undergraduate and postgraduate degrees in human genetics from the University of Stellenbosch. During her Ph.D., Natalie studied the genetic factors that regulate iron metabolism using state-of-the-art molecular techniques and bioinformatics.
After completing her Ph.D., she undertook a five-year post-doctoral research fellowship at the Institute for Infectious Disease and Molecular Medicine at the University of Cape Town. Natalie’s area of expertise was infectious disease immunology with a close interest in cellular immunity to HIV and TB co-infection.
She has extensive experience in both molecular and advanced immunological techniques, including multi-parameter flow cytometry.
About Synexa Life Sciences BV
Synexa is an industry leader in contract bioanalytics and biomarker research services specializing in biopharmaceuticals, supporting Biopharma partners across the globe to achieve their clinical milestones with bespoke analytical solutions to meet specific challenges. Our global purpose-built laboratories have been designed and fitted to meet the fast-changing and ever-evolving complexity of drug development pipelines.
Guided by a combined scientific experience of over 800 years, our team of world-class scientists pride themselves on going the extra mile to deliver high levels of customer service and quality science that meets your expectations. We specialize in providing quality scientific expertise in key disease areas, encompassing a wide range of technology platforms and bespoke assay solutions to meet each outcome.
Services include protein, cell and gene therapy bioanalytics, biomarker discovery, analysis and validation, PK/PD, de novo assay method development and validation, and ProtoTrials®, our proprietary human in vivo translational research platform focused on providing valuable early clinical insights.