In a recent study published in the U.S. Centers for Disease Control and Prevention journal Emerging Infectious Diseases, researchers described an unusual case of patient-to-healthcare worker (HCW) monkeypox virus (MPXV) transmission via a needlestick injury that occured in Brazil.
 Research Letter: Monkeypox Virus Transmission to Healthcare Worker through Needlestick Injury, Brazil. Image Credit: FOTOGRIN / Shutterstock
Research Letter: Monkeypox Virus Transmission to Healthcare Worker through Needlestick Injury, Brazil. Image Credit: FOTOGRIN / Shutterstock
Background
A recent study reported only one case of MPXV transmission in healthcare facilities to an HCW, likely through contact with contaminated bedding. Earlier, nonendemic countries had only sporadic zoonotic or travel-associated monkeypox outbreaks. Human-to-human or animal-to-human MPXV transmission was rare even in Africa before 2022. However, during May–September 2022, over 64,000 MPXV cases worldwide, mainly via sexual contact, were recorded.
About the study
In the present study, researchers described clinical features of MPXV infection in a 20-year-old female nurse after a needlestick injury she sustained on July 9, 2022. The nurse was collecting discardable materials wearing personal protective equipment (PPE) when a needle perforated her glove; the puncture site was evident immediately. The researchers collected blood, skin lesion samples, and oropharyngeal samples from the infected nurse to test for MPXV deoxyribonucleic acid (DNA).
The source of MPXV infection was a 20-year-old male patient. Two weeks before the needlestick incident, he contracted a mild monkeypox infection. His clinical symptoms encompassed pain in the throat, cervical lymphadenopathy, and skin lesions on the face, torso, and groin. The authors received consent from both the patient and nurse for this report.
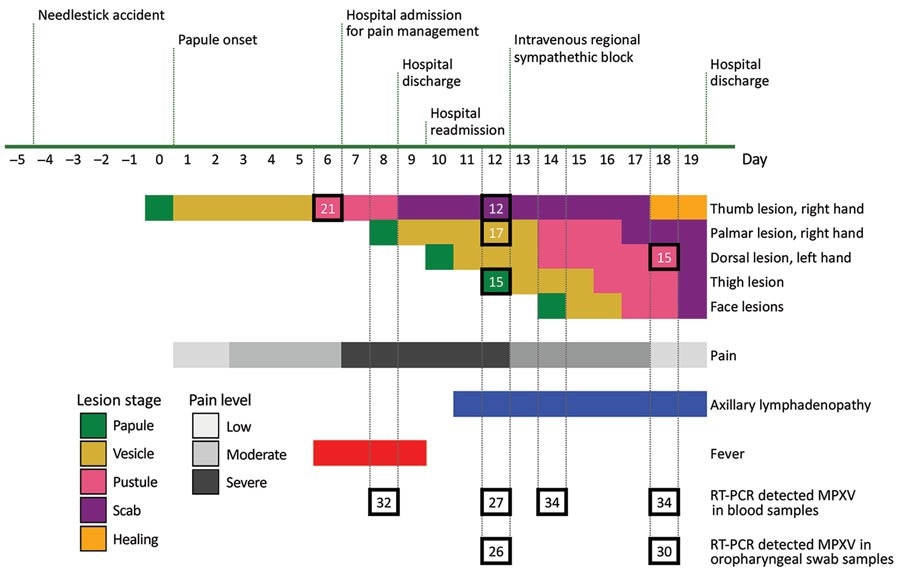
Timeline of symptoms and testing in a case of MPXV transmission to healthcare worker through needlestick injury, Brazil. All collected specimens had RT-PCR detectable MPXV through hospital discharge. Numerals inside squares indicate RT-PCR cycle threshold values. MPXV, monkeypox virus; RT-PCR, reverse transcription PCR.
Study findings
All the specimens collected from the nurse had detectable MPXV DNA during the entire duration of hospitalization, yet, she was transferred into outpatient care before lesion resolution. This case gave a much-needed sneak peek into the natural progression of MPXV infection by enabling the researchers to study clinical and laboratory results of different disease stages. MPXV, in this case, had an incubation period of five days. First, the patient experienced pain and inflammation at the injury site and then developed a cutaneous lesion. General disease symptoms, including fever and lymphadenopathy, appeared later.
Concerning the number of skin lesions, the nurse had seven lesions, with three on her face, one on the thumb (inoculation site), right-hand palm, left-hand dorsal side, and left thigh. Magnetic resonance imaging (MRI) of her injury site on day 15 showed a neurovascular bundle and subcutaneous inflammation. Furthermore, the authors noted that the unusual needlestick MPXV transmission abrogated a prodromal phase in the HCW. It was similar to bite or scratch MPXV transmission from infected animals to humans.
Most patients who acquire MPXV by sexual contact have severe anorectal pain. Likewise, the nurse experienced severe injury site pain, indicating that painful lesions and neural impairment begins at the primary MPXV inoculation site, as observed in the nurse's MR images. Moreover, the researchers detected MPXV DNA in the nurse's blood sample on day 8 of infection, before the appearance of skin lesions at distant sites, indicating hematogenous MPXV dissemination. Another retrospective study of MPXV antiviral therapy similarly detected MPXV DNA in a patient's blood after 14 days, after skin lesions had resolved.
There is no explanation of how detectable MPXV DNA correlates with true viremia. However, persistent detection of MPXV DNA points to its bloodborne transmission via needlesticks, blood transfusions, and organ transplants. The authors also consistently detected viral DNA in the oropharyngeal samples of HCW, although the efficiency of the droplet or airborne transmission of MPXV remains unknown.
Conclusions
Due to a scarcity of documented cases of needlestick monkeypox transmission, the researchers could not comment on MPXV transmission risk. However, this case points out that instruments used on cutaneous lesions likely pose a high risk. Smallpox vaccination was discontinued in Brazil after 1979, and smallpox or monkeypox vaccines are unavailable in Brazil as yet. The World Health Organization (WHO) recommends pre-and post-exposure prophylaxis, including vaccination of HCWs on priority with a second or third-generation vaccine (when available). Notably, a vaccine against MPXV could be given even after four days of viral exposure.
Journal reference:
- Monkeypox Virus Transmission to Healthcare Worker through Needlestick Injury, Brazil, Laína Bubach Carvalho, Luciana V.B. Casadio, Matheus Polly, Ana Catharina Nastri, Anna Cláudia Turdo, Raissa H. de Araujo Eliodoro, Ester Cerdeira Sabino, Anna Sara Levin, Adriana Coracini Tonacio de Proença, and Hermes Ryoiti Higashino, Emerg Infect Dis. 2022, DOI: https://doi.org/10.3201/eid2811.221323, https://wwwnc.cdc.gov/eid/article/28/11/22-1323_article