Children and adolescents with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection experience a milder course than adults and recover within a few weeks. The definition of a symptom varies; therefore, there is inconsistent reporting of persistent symptoms, which can last for several months after infection and range from 0% to 66%. The fact that there are more unbiased results on post-acute sequelae and symptoms among younger patients further complicates these conclusions. The nature, frequency, and definition of post-acute sequelae in children and adolescents are still unknown, and there is a discrepancy between the clinical appearance and objective findings.
Study: Pulmonary Dysfunction after Pediatric COVID-19. Image Credit: MarcinWojc / Shutterstock
About the study
In the present study, researchers described the morphologic and functional changes in the lung parenchyma on low-field magnetic resonance imaging (MRI) in post-COVID-19 children and adolescents compared to healthy controls.
The team conducted a cross-sectional, investigator-initiated experiment between August 2021 and December 2021 at a single academic medical facility to examine lung parenchymal abnormalities in adolescents and children after SARS-CoV-2 infection. From a nationwide search, the study enrolled consecutive patients with COVID-19. A blood sample was collected, and all subjects with COVID-19 and healthy controls underwent low-field MRI after being evaluated for clinical criteria. Imaging data were compared with clinical characteristics before and after infection, the time since a positive reverse transcription–polymerase chain reaction (RT-PCR) test, and laboratory values.
The COVID-19 group's inclusion requirements included the requirement to be between five and 18 years old. RT-PCR testing for SARS-CoV-2 was necessary for all eligible patients, regardless of the duration between the positive test and trial enrollment. The healthy control group's inclusion requirements included a specified age range of five and 18 years.
In the study, long COVID was defined as having symptoms that persisted for at least 12 weeks and met one of the four criteria listed below: (1) Symptoms that persisted after the acute COVID-19 phase or its treatment, (2) symptoms that triggered a new health restriction, (3) new symptoms that appeared after the acute phase but were recognized as a result of COVID-19 disease, and (4) worsening of pre-existing comorbidity.
Using low-field proton MRI, the primary result found was the frequency of morphological alterations in the lung parenchyma. Secondary outcomes included laboratory evaluations, reported clinical complaints, functional lung changes including ventilation defects, perfusion defects, and the match and defect of both.
The medical histories of COVID-19 group participants and their symptoms both during and after COVID-19 infection were evaluated. Each person measured their blood pressure and heart rate. Blood was drawn to measure the blood count, interleukin (IL)-6, C-reactive protein (CRP), and antibodies against SARS-CoV-2 spike protein and nucleocapsid antibodies.
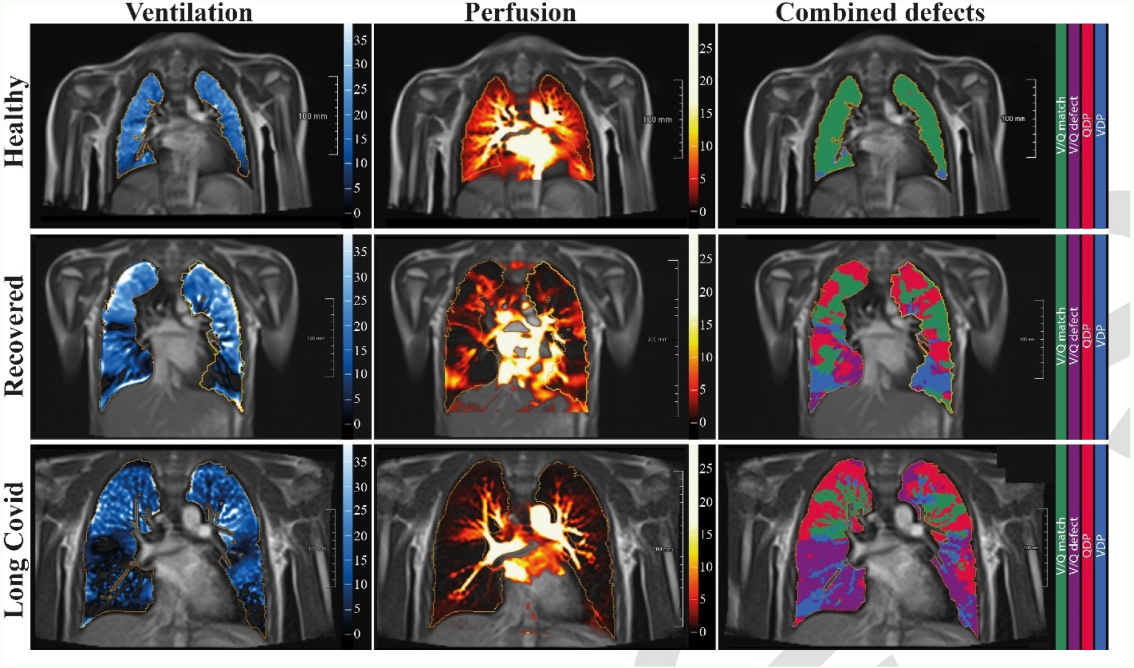
Free-breathing phase-resolved functional lung (PREFUL) low-field MRI at 0.55T with calculated parameters at an axial plane after automatic registration to a mid-expiration position and lung parenchyma segmentation. From left to right, representative color-coded images of functional show ventilation defects (VDP, blue), perfusion defects (QDP, red), ventilation/perfusion (V/Q match, green), ventilation/perfusion defects (V/Q defect, purple) in a healthy control (upper row, 7-year-old male), a participant recovered from COVID-19 (middle row, 10-year-old male) and a participant with long COVID (15-year-old male).
Results
Almost 91 pediatric patients with RT-PCR-positive SARS-CoV-2 infection and 17 healthy controls in total were screened. After exclusions, clinical, laboratory, and low-field MRI examinations were completed by 54 people with post-acute COVID-19 and nine controls.
Both groups' individuals had a lot of the same traits. Participants with post-acute COVID-19 had a mean age of 123 years, a mean weight of 4818 kg, a mean height of 15617 cm, and 44% of them were female. A total of 54 people received RT-PCR results for SARS-CoV-2 infection. Among these, 54% had recovered, and 46% were categorized as having long-COVID.
In addition to shortness of breath, 9% of the participants experienced headache, 28% had dyspnea, 2% had pneumonia, 7% had anosmia, 2% reported ageusia, 7% had fatigue, 11% had impaired attention, and 2% experienced limbic pain. In 22% of the healthy volunteers, 5% of the recovered patients, and 10% of the long COVID-19 patients, pre-existing diseases were found. During the acute phase of the infection, four subjects with RT-PCR-positive SARS-CoV-2 infection did not exhibit any symptoms.
Only one participant in the recovered group out of the 54 people in the post-acute COVID-19 group and the nine healthy controls who underwent low-field MRI scanning showed any morphological alterations. Using functional In press low-field MRI, greater ventilation, perfusion, and combination deficits were discovered in diseased individuals compared to healthy controls. Comparing the post-COVID group to healthy controls, the ventilation/perfusion match (V/Q match) was poorer in the post-COVID group.
The overall ventilation defect percentage (VDP) was higher in the recovered or the long-COVID group than in the healthy controls when the COVID-19 group was divided by clinical characteristics. Like the recovered group, the long-COVID group's perfusion defect percentage (QDP) was higher than the healthy controls. Compared to the recovered and long COVID groups, combined V/Q deficiencies were smaller in healthy controls. Similar to the V/Q match, the healthy controls had a greater ratio than the recovered and long COVID groups.
Overall, the study reported the ongoing pulmonary dysfunction observed on low-field MRI in adolescents and children with long COVID and those who have recovered from COVID-19.
Journal reference:
- Pulmonary Dysfunction after Pediatric COVID-19, Rafael Heiss, Lina Tan, Sandy Schmidt, Adrian P. Regensburger, Franziska Ewert, Dilbar Mammadova, Adrian Buehler, Jens Vogel-Claussen, et.al, 2022/09/20, Radiology, 221250, Radiological Society of North America, DOI: https://www.doi.org/10.1148/radiol.221250, https://pubs.rsna.org/doi/10.1148/radiol.221250