Human physiological processes rely heavily on sleep for proper functioning. A recent PLOS Medicine journal study determined the relationship between sleep duration of older people, i.e., 50, 60, and 70 years of age, and the incidence of multimorbidity. Significantly, the study utilized follow-up data for twenty-five years for the analysis.
Although several studies have indicated the relationship between sleep duration and the manifestation of chronic diseases (e.g., cancer and cardiovascular disease) and mortality, the nature of this association remains unclear.
When more than one chronic condition prevails within the same individual, it is known as multimorbidity. However, not many studies are available regarding the association between multimorbidity and sleep duration. Additionally, whether sleep duration impacts health, manifests chronic conditions, and subsequent mortality is not known.
Currently, older adults are recommended 7 to 8 hours of sleep; however, whether short or long sleep duration increases the risk for morbidity should be explored in future research. The underlying biological mechanisms associated with short-duration sleep and the onset of comorbidities are available; however, the impact of extended sleep on the manifestation of chronic conditions is not well understood.
It has been reported that as an individual gets older, the sleep pattern changes. Hence, the question arises if changes in sleep patterns in mid or later-life increase the risk of multimorbidity.
About the Study
The current research utilized the Whitehall II cohort, an ongoing study established in 1985 comprising 10,308 (6,895 men and 3,413 women) British civil servants. Since 99.9% of the participants were linked to UK National Health Service (NHS) electronic health records, relevant medical data were obtained from this service.
Self-reported information on the average week-night sleep duration of the participants was obtained at six data collection waves between 1985 and 2016. This information was categorized based on age, i.e., 50, 60, and 70 years of age. Jenkins's sleep problems scale was used to assess sleep quality. Participants were asked about their sleep experiences, such as troubled sleep, disturbed sleep, waking up several times at night, and difficulty falling asleep.
In this study, multimorbidity was defined as the presence of two or more chronic diseases out of thirteen identified based on the Whitehall clinical examinations up to March 2019.
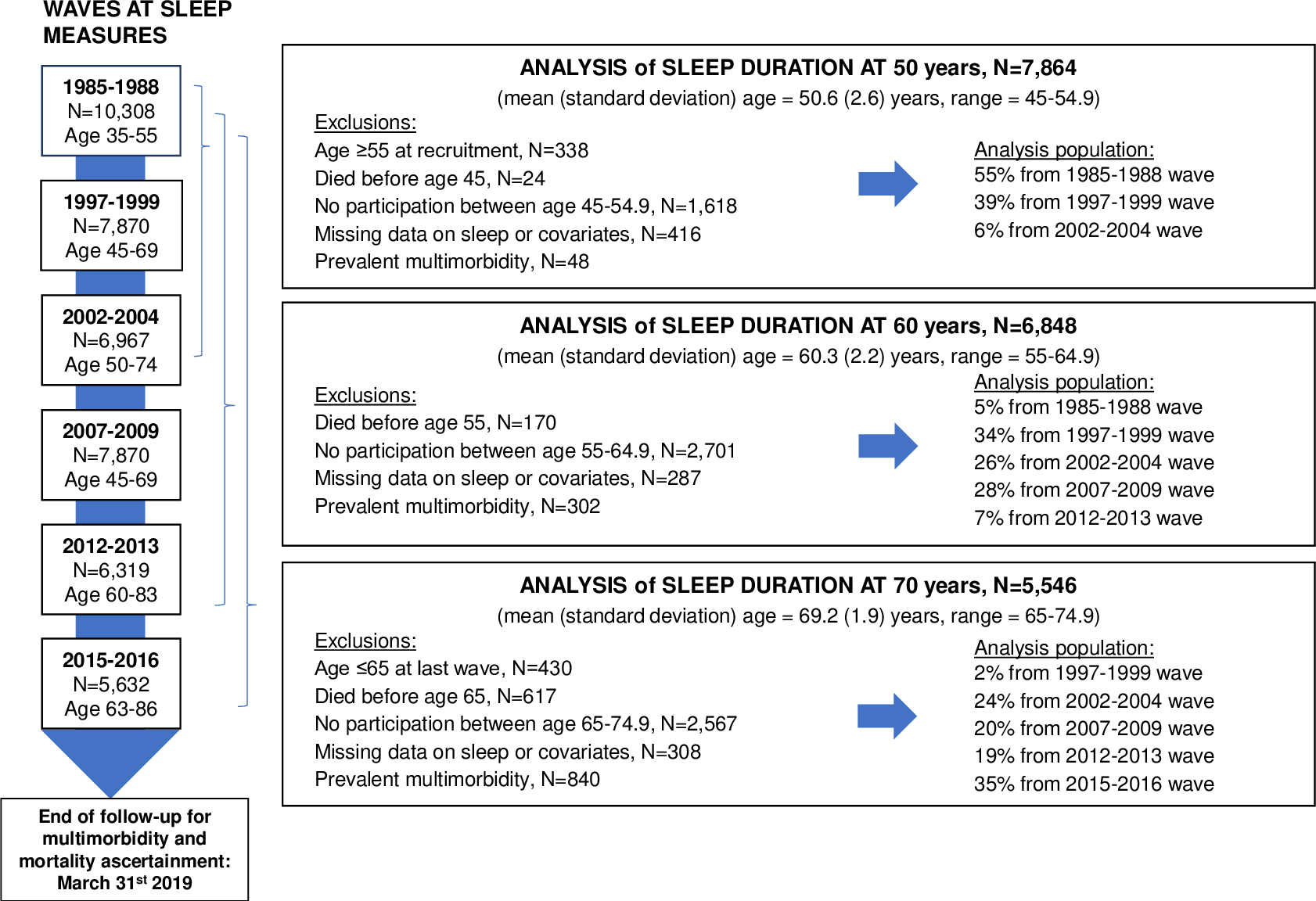 Flowchart for analyses on the association between sleep duration at age 50, 60, and 70 and risk of multimorbidity.
Flowchart for analyses on the association between sleep duration at age 50, 60, and 70 and risk of multimorbidity.
Study Findings
A total of 7,864 participants who did not have multimorbidity were at the age of 50 years. Among this group, 4,446 developed the first chronic disease, 2,297 progressed to multimorbidity, and 787 subsequently died.
It was observed that compared to seven hours of sleep, those who slept less than five hours at 50 years showed an increased risk of developing their first chronic disease. Interestingly, sleep duration above nine hours was not associated with such transitions.
The current prospective study presented three key findings. First, short sleep duration was constantly linked to an increased multimorbidity risk. This observation was accurate for both middle-aged and older age group participants. Short sleep duration was also associated with first disease onset and subsequent multimorbidity. However, it was not linked with mortality.
Second, long sleep duration was less likely at 60 and 70 years of age, and an incidence of multimorbidity was observed. However, this was not true for participants who were 50 years of age. Hence, long sleep duration at 50 years of age was not associated with disease progression.
Third, the accelerometer-based sleep duration measurement undertaken in participants whose mean age was 69 years confirmed the relationship between the sleep duration and incidence of multimorbidity at ages 60 and 70.
Strengths and Limitations
The major strengths of this study include the long follow-up period and repeated measurement of sleep duration of varied age groups. Furthermore, using multistate models provided more insight into the association of sleep duration with the course of the disease.
A fundamental limitation of this study is the small number of participants in the long sleep duration category. As a result, the authors failed to conduct inference in this group regarding the incidence of multimorbidity. Additionally, the self-reporting nature of the study increased the risk of biased results. The authors also indicated the risk of reverse causality from undiagnosed conditions at sleep measures. The cohort contained a limited number of non-white participants, so the findings could not be generalized.
Conclusions
The current study strongly indicated the relationship between short sleep duration and the development of multimorbidity. This observation is accurate for individuals in their mid or late life. Short sleep duration at age 50 was linked with a higher risk of first chronic disease onset and subsequent multimorbidity. The current study recommended good sleep duration and quality for better health outcomes.