As of November 29, 2022, the World Health Organization (WHO) has announced that the monkeypox virus will now be referred to as “mpox” in an effort to reduce the stigmatization of this condition.
Since the start of the current mpox outbreak in numerous non-endemic regions throughout the world, racist and stigmatizing language and have been widely spread on social media platforms. Following the increasing number of concerns raised by many individuals and countries over this issue, the WHO, under the International Classification of Diseases (CID) and the WHO Family of International Health Related Classifications, recommended the adoption of “mpox” to replace the use of “monkeypox” in WHO communications.
Removing ‘monkey’ removes the stigma that monkeypox comes with and deals with the possible misinformation.”
The current status of the mpox outbreak
Over 81,000 cases of mpox virus infection have been reported worldwide in 110 different locations, 103 of which are non-endemic areas.
The mpox virus, an Orthopoxvirus with manifestations similar to smallpox infection, usually is endemic to central and west African countries. However, in April of this year, several new mpox cases were reported in other areas of the world, many of which were documented in men who have sex with men (MSM).
Mpox symptoms and transmission
Symptoms will begin to develop about three weeks after being infected with the mpox virus. The most common mpox infection symptom is a rash located on or near the genitals and anus and other areas of the body, including the hands, feet, chest, face, or mouth. The pimple/blister-like appearance of the mpox rash will eventually scab before healing.
In addition to a rash, mpox infection may cause fever, chills, swollen lymph nodes, fatigue, muscle aches, headache, and respiratory symptoms, including a cough, sore throat, or nasal congestion.
The most common way mpox is transmitted is through skin-to-skin contact with an infected individual, such as sexual intercourse, hugging, kissing, or prolonged face contact. In addition to this transmission route, the mpox virus can also be transmitted following contact with contaminated objects, fabrics, and surfaces previously used by an infected individual.
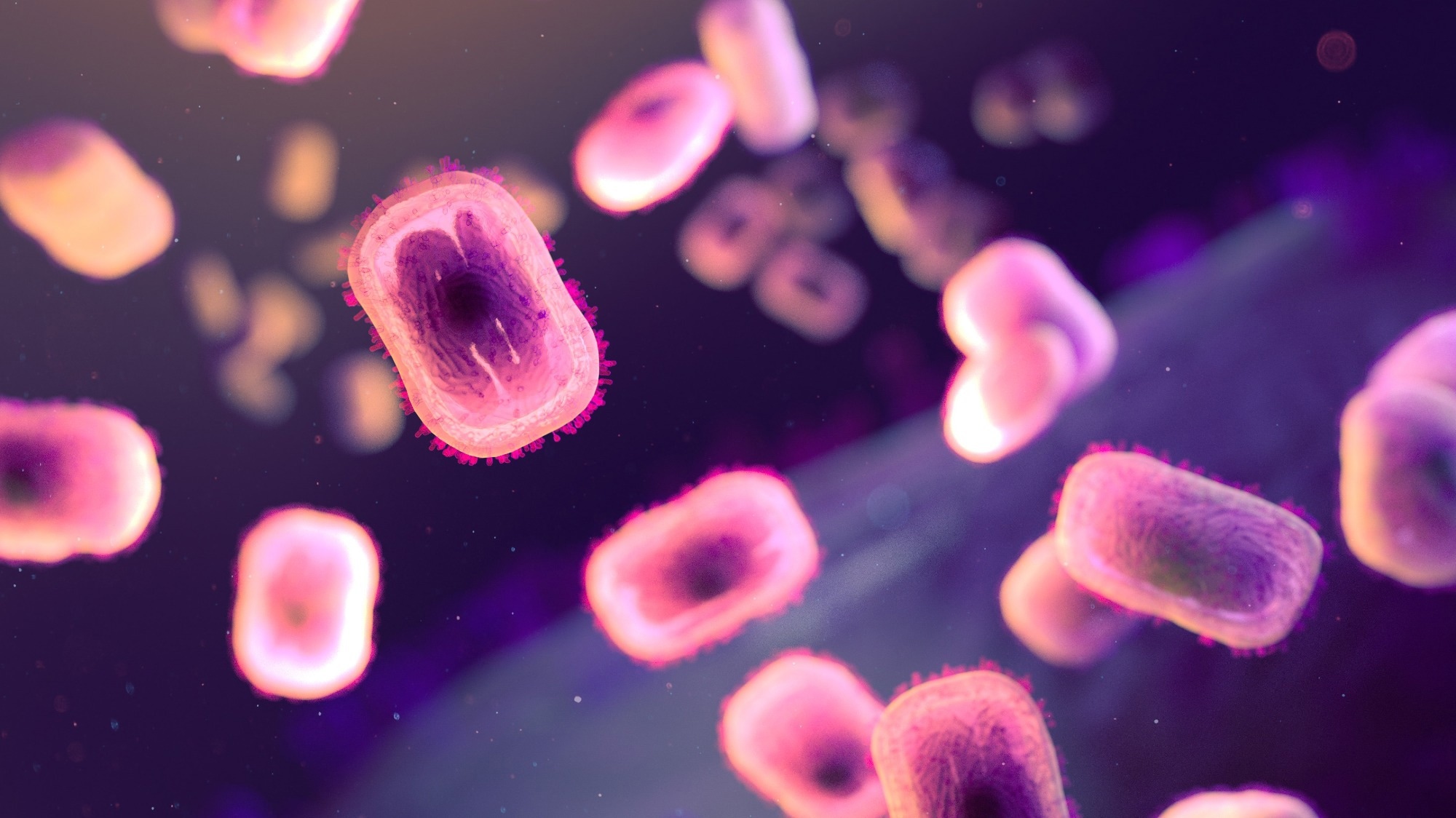
Extracellular, brick-shaped mpox virions (colorized pink). Backlighting shows the surface membranes of the virions and the outlines of nucleocapsids. Credit: NIAID.
Vaccines
In the United States, the JYNNEOS and ACAM2000 vaccines have been approved to prevent the spread of the mpox virus due to the structural similarities between the mpox and smallpox viruses. Individuals previously exposed to a mpox-infected individual will likely be exposed to mpox in the future or are immunocompromised and are advised to receive either vaccine to prevent infection.
Treatments
Importantly, no specific mpox antiviral agents have been approved for use; however, antiviral agents initially developed for treating smallpox infection may also be effective in treating mpox infection. Only those currently experiencing severe forms of mpox infection or are considered high risk for severe disease are eligible to receive these treatments.
Tecovirimat, for example, is considered the first line of therapy for treating at-risk patients with mpox infection. This antiviral medication is typically administered as a prophylactic measure to exposed individuals with severe immunodeficiency in T-cell function and would otherwise not be eligible to receive smallpox/mpox vaccination.
Brincidofovir, otherwise known as Tembex, is another smallpox drug available for treating mpox infections in adults. Only mpox-positive individuals experiencing severe disease or are at risk of severe infection can receive this drug.
In addition to these agents, vaccinia immune globulin intravenous (VIGIV) and cidofovir are other therapeutic modalities that may be employed in treating mpox infection.