Fatty foods harm our health. Prior research has established a link between the consumption of dietary fats and non-alcoholic fatty liver disease, which subsequently leads to inflammation and tumor formation in the liver. However, the precise effects of dietary fat composition on liver tumorigenesis remain elusive. A new study shows that dietary saturated/trans fats, but not cholesterol, can induce hepatic angiogenesis and lymphangiogenesis, key drivers of tumorigenesis, in hepatitis C virus core gene transgenic mice.
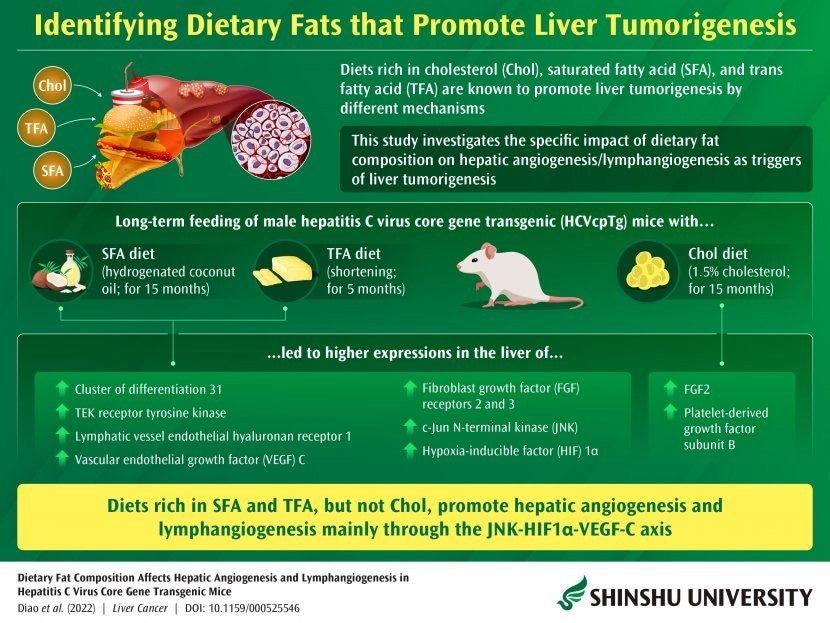
Image Credit: Shinshu University
In light of the recent pandemic, people across the globe are increasingly becoming aware of the importance of consistent high-quality nutrition and daily exercise. Multiple studies have already demonstrated the positive and negative effects of various dietary constituents on human health. More specifically, prior studies conducted on certain types of transgenic mice have shown that fat-rich diets comprising trans-fatty acid (TFA), saturated fatty acid (SFA), and cholesterol cause non-alcoholic fatty liver disease, which may then promote inflammation and tumor formation in the liver. However, the precise effects of dietary fat compositions have remained unknown so far.
Researchers led by Professor Naoki Tanaka from the Department of Global Medical Research Promotion, Shinshu University Graduate School of Medicine, Japan, have recently endeavored to fine-tune previous findings and fill in this gap in knowledge. Using experiments involving transgenic mice, they have successfully shown that dietary saturated/trans fats, but not cholesterol, can trigger hepatic angiogenesis and lymphangiogenesis, leading to the promotion of hepatic tumors. Angiogenesis (the formation of new blood vessels) and lymphangiogenesis (formation of new lymphatic vessels), i.e., neovasculogenesis, are key determinants for the survival, proliferation, and metastasis of cancer cells.
Dietary TFA, SFA, and cholesterol are present in a variety of food sources. For instance, cholesterol is abundant in animal-derived foods like eggs, cheese, shellfish, meats, sardines, and full-fat yogurt. Whereas SFA is primarily found in animal and plant products such as red meat, dairy items, palm oil, and coconut oil, TFA naturally occurs in dairy products and animal meat in relatively smaller amounts. Certain products, such as partially hydrogenated vegetable oils, contain relatively larger amounts of TFA."
Professor Naoki Tanaka, Department of Global Medical Research Promotion, Shinshu University Graduate School of Medicine, Japan
To study the association between dietary fat composition and liver neovasculogenesis, the researchers fed hepatitis C virus core gene transgenic (HCVcpTg) mice with a control diet or with TFA-/SFA-/cholesterol-rich diets containing the same number of calories. The cholesterol diet comprised ingredients with 1.5% cholesterol, the SFAs were derived from hydrogenated coconut oil, and the TFA diet consisted of shortening. The researchers then monitored the degree of hepatic angiogenesis and lymphangiogenesis and growth factor expression using a variety of techniques including quantitative mRNA measurement, immunoblot analysis, and immunohistochemistry. They reported their findings in an article that was made available online on 16 September 2022 and subsequently published in Liver Cancer.
Says Prof. Tanaka, "Long-term feeding of SFA and TFA diets to HCVcpTg mice increased the expressions of vascular endothelial cell indicators like CD31 and TEK receptor tyrosine kinase, in addition to lymphatic vessel endothelial hyaluronan receptor 1. We also detected elevated levels of vascular endothelial growth factor C and fibroblast growth factor receptors 2 and 3, as well as c-Jun N-terminal kinase and hypoxia-inducible factor 1α in the mice livers." Incidentally, vascular endothelial growth factor C (VEGF-C), fibroblast growth factor (FGF) receptors 2 and 3, c-Jun N-terminal kinase (JNK), and hypoxia-inducible factor (HIF) 1α are important biomolecules involved in cell communication and growth signaling. JNK-HIF1α-VEGF-C axis and FGFs are thus powerful drivers of hepatic neovasculogenesis.
What does this information translate to? Increased formation of new blood and lymphatic vessels in the liver.
But this may not necessarily be bad news. According to Prof. Tanaka, "We demonstrated for the first time that hepatic angiogenesis and lymphangiogenesis were enhanced by saturated-fat- or trans-fat-rich diets, but not cholesterol-rich diets, mainly through the JNK-HIF1α-VEGF-C axis. These processes are crucial targets for treating hepatocellular carcinoma."
He further adds: "Agents inhibiting hepatic angiogenesis are widely used for treating hepatocellular carcinoma. However, I also recommend avoiding fatty-acid-rich diets especially if someone is at a high risk of developing liver cancer or undergoing treatment for liver cancer."
Besides monitoring our food intake, the researchers also recommend developing newer methods of food production that can significantly decrease the generation of trans-fatty acids in foods. This, based on their observations in this study, is in keeping with the World Health Organization's call for global elimination of industrially-generated trans-fatty acids from our food supplies by 2023 under the "REPLACE" action package.
Saying no to French fries may not be that easy, but in the interest of our hepatic health, we may just have to, thanks to these insightful findings by the researchers of Shinshu University.
Source:
Journal reference:
Diao, P., et al. (2022) Dietary Fat Composition Affects Hepatic Angiogenesis and Lymphangiogenesis in Hepatitis C Virus Core Gene Transgenic Mice. Liver Cancer. doi.org/10.1159/000525546.