The ongoing coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), continues to affect the already overburdened healthcare system.
For example, the pandemic aggravated the cancer-related healthcare crisis, as most resources were reallocated to manage SARS-CoV-2-infected patients. As a result, the waiting time to obtain non-COVID-19-related healthcare services increased substantially.

Study: Healthcare in England was affected by the COVID-19 pandemic across the pancreatic cancer pathway: a cohort study using OpenSAFELY-TPP. Image Credit: Ground Picture / Shutterstock.com

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Background
During the pandemic, patients’ behaviors towards seeking healthcare services changed, as they opted for social distancing to protect themselves. People were also very cautious about the unprecedented pressure on healthcare personnel during the pandemic, which led to widespread social distancing to limit the spread of SARS-CoV-2. These changes affected cancer patients, as they heavily depend on healthcare services.
The diagnosis of pancreatic cancer requires an efficient system, as it presents non-specific symptoms. Some of the symptoms associated with this type of cancer include diabetes, bile duct obstruction, weight loss, and hyperglycemia.
The timely assessment of glycated hemoglobin (HbA1c), liver function, and body mass index (BMI) aids in the early diagnosis and monitoring of the disease progression. The tremendous pressure on the healthcare system during the pandemic resulted in cancer treatment delays, which invariably affected disease prognosis.
To mitigate these negative effects of the pandemic, the first step is to assess the scale of the impact. A new study published on the medRxiv* preprint server investigates the impact of the COVID-19 pandemic on pancreatic cancer services in England.
About the study
One of the objectives of the current study was to assess the impact on a wide range of services, such as diagnostics, treatment, and outcomes. The authors determined the number of healthcare services that could be provided if the COVID-19 pandemic had not occurred. The pattern of recovery from the healthcare services, post-pandemic, was also assessed.
Electronic healthcare records (EHR) of adults with pancreatic cancer, based in England, were analyzed. All participants were diagnosed between January 1, 2015, and September 30, 2022.
In this study, the nationally representative OpenSAFELY-TPP dataset was used, which consisted of records of 24 million people, which is approximately 40% of the population of England. OpenSAFELY is an analytical platform that addresses urgent COVID-19 research questions.
Study findings
During the pandemic, several pancreatic cancer-related services were disrupted across the treatment pathway. This finding is consistent with a previous study that reported the adverse effect of the pandemic on healthcare services.
Healthcare assessments including BMI, HbA1c, and liver function were provided to a smaller number of patients as compared to pre-pandemic rates. This suggests that the COVID-19 pandemic affected the early diagnosis of pancreatic cancer, along with the diagnosis of other diseases such as diabetes. This could also affect the quality of routine data for research.
Importantly, it was observed that even two and a half years into the pandemic, pre-pancreatic cancer diagnosis testing did not recover to pre-pandemic levels. Nevertheless, those who were diagnosed with pancreatic cancer received proper care.
It was also observed that individuals who were already diagnosed with pancreatic cancer prior to the pandemic experienced an initial drop in receiving the aforementioned routine tests; however, the levels recovered by the sixth month of the pandemic.
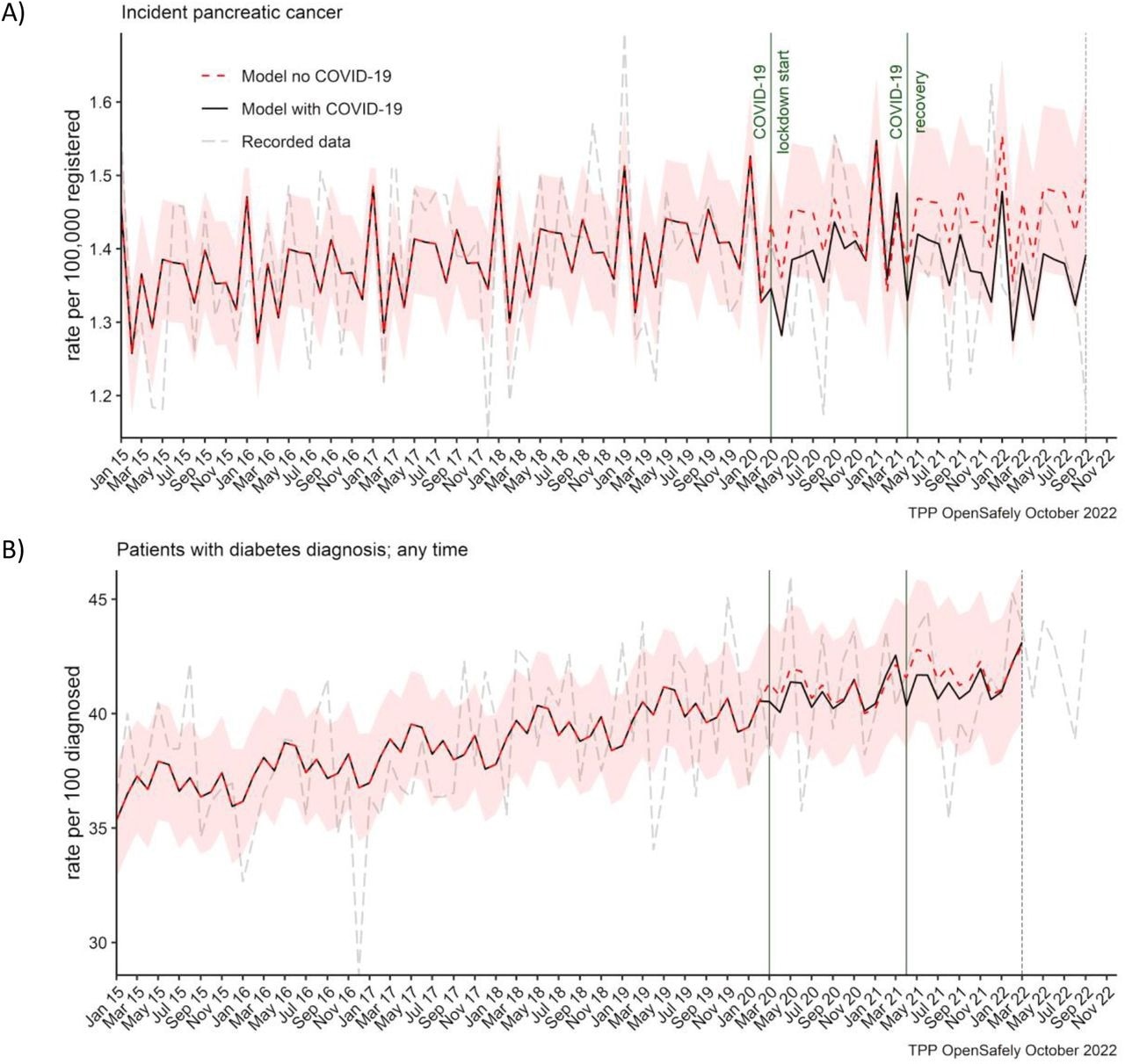 Observed and predicted monthly rates (as if the COVID-19 pandemic had not happened) for A) pancreatic cancer diagnosis per 100,000 registered patients, and B) diabetes diagnosis per 100 people with pancreatic cancer.
Observed and predicted monthly rates (as if the COVID-19 pandemic had not happened) for A) pancreatic cancer diagnosis per 100,000 registered patients, and B) diabetes diagnosis per 100 people with pancreatic cancer.
Although previous studies reported the suspension of many non-emergency diagnostic services such as abdominal imaging during the first wave of the pandemic, this was soon restored following infection control guidelines.
Unlike other types of cancer, such as breast, kidney, and colorectal, the current study observed that the diagnosis of pancreatic cancer and diabetes was not significantly affected. This is because the diagnosis of both these diseases does not depend on screening programs and diagnostic services in primary care.
These findings contradicted earlier studies, which reported that the diagnosis of diabetes was delayed due to the adverse effect of the pandemic on the healthcare system.
Strengths and limitations
A key strength of the current study is the OpenSAFELY-TPP dataset, which represents a large-scale population. Notably, the study design enabled assessment of the COVID-19 pandemic on a particular disease, instead of already known effects on the general healthcare services.
Analysis of the large dataset provided a less-biased estimate of the effect of the pandemic. The key limitation of the study centered around the use of clinical codes to extract data, which increased the risk of missing important information or miscoding.
Conclusions
It is imperative to monitor the burden on healthcare services to ensure good service quality. A regular assessment would also help determine the extent of recovery from the pandemic crisis state.
Furthermore, it is also important to learn from resilient healthcare services, which continued to provide uninterrupted services throughout the pandemic, by implementing novel strategies.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Lemanska, A., Andrews, C., Fisher, L., et al. (2022). Healthcare in England was affected by the COVID-19 pandemic across the pancreatic cancer pathway: a cohort study using OpenSAFELY-TPP. medRxiv. doi:10.1101/2022.12.02.22283026. https://www.medrxiv.org/content/10.1101/2022.12.02.22283026v1.
- Peer reviewed and published scientific report.
Lemanska, Agnieszka, Colm Andrews, Louis Fisher, Ben Butler-Cole, Amir Mehrkar, Keith J. Roberts, Ben Goldacre, Alex J. Walker, and Brian MacKenna. 2023. “A National Audit of Pancreatic Enzyme Prescribing in Pancreatic Cancer from 2015 to 2023 in England Using OpenSAFELY-TPP.” Seminars in Oncology Nursing, May, 151439. https://doi.org/10.1016/j.soncn.2023.151439. https://www.sciencedirect.com/science/article/pii/S0749208123000761.