
 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Background
The current study used COVID-19 vaccination and gross domestic product (GDP) per capita data from 160 countries. By June 2022, 97 of these 160 countries had vaccinated nearly half of their population. However, the global COVID-19 vaccine supply was unequal, with high-income countries receiving more vaccines than low- and middle-income countries.
Thus, there is a need to increase vaccine supplies to countries with lower availability while incorporating racial and socioeconomic aspects to devise a prioritization strategy. It is also essential to understand the extent of heterogeneity in COVID-19 vaccination temporal trends across and within countries and its impact on disease outcomes.
About the study
COVID-19 vaccination temporal dynamics were considered in 160 countries and territories and over 8,000 subnational locations. Of these areas, publicly available temporal vaccination data was retrieved from 34 countries and territories that had vaccinated at least 50% of their population with a first dose. In addition, data from 12 sub-national localities were also included in the final SES-based analysis.
These 12 sub-national localities were categorized into quantiles based on measures representing SES, such as poverty rates. Finally, the degree of SES disparity was determined using the ratio and difference for the median, maximum, and percentage of the population vaccinated in the final study week.
Any biases of the quantile-based analysis due to the relative inequality within each location were identified. The Lorenz curves for 83 of the total areas evaluated in this study were constructed to estimate a corresponding Gini coefficient of vaccine inequality.
Results
Socioeconomic disparities existed in a large proportion of vaccinated individuals within each country and between many countries. Moreover, the inequity in vaccine administration remained in favor of high SES groups in most countries and territories, a trend that did not change over time. In addition, the inequitable vaccine distribution trend exhibited a wide range of Gini values.
Quantile-based analysis discerned SES-stratified temporal trends in COVID-19 vaccination for 81 places, spanning 26 countries with varying national GDP per capita. These trends were identified in 33 and 24 states of the United States of America and Brazil, respectively.
![SARS-CoV-2 vaccine coverage. (A) Association between population vaccinated with at least one dose and gross domestic product (GDP) per capita for 160 countries and territories. Vaccine and population data come from [23–55] and were compiled by the Financial Times as of June 22, 2022. GDP data are sourced from World Bank [56] and PCBS [57]. (B) Sub-national vaccination data resolution. Based on publicly available data for places with 50% or more of their population vaccinated with at least one dose, we identified 7 countries/territories with vaccination rates for 100 or more locations, 17 for 21-99, and 10 for 12-20 locations. In this study, we excluded 78 countries that have greater than 50% vaccination coverage due to a lack of high-resolution sub-national data, which are referenced as ‘not included’ in the legend. Details of the data sources and dates of data collection are reported in tables S1 and S2, respectively.](https://www.news-medical.net/images/news/ImageForNews_740402_16777228277199513.jpg)
SARS-CoV-2 vaccine coverage. (A) Association between population vaccinated with at least one dose and gross domestic product (GDP) per capita for 160 countries and territories. Vaccine and population data come from [23–55] and were compiled by the Financial Times as of June 22, 2022. GDP data are sourced from World Bank [56] and PCBS [57]. (B) Sub-national vaccination data resolution. Based on publicly available data for places with 50% or more of their population vaccinated with at least one dose, we identified 7 countries/territories with vaccination rates for 100 or more locations, 17 for 21-99, and 10 for 12-20 locations. In this study, we excluded 78 countries that have greater than 50% vaccination coverage due to a lack of high-resolution sub-national data, which are referenced as ‘not included’ in the legend. Details of the data sources and dates of data collection are reported in tables S1 and S2, respectively.
Two distinct temporal COVID-19 vaccination trend,s including concave or sigmoidal type,s were found to vary widely in shape and vaccination rollout speed. The concave dynamic trend, associated with a faster initial vaccine rollout, plateaued rapidly but averted more COVID-19 cases and deaths, while the latter was initially slow.
Note that the time of vaccine rollout was not associated with the GDP per capita of the country. For example, Cape Verde implemented a faster initial COVID-19 vaccination rollout campaign than many high-GDP countries, such as Belgium.
Modulating the vaccination rollout time early on could be beneficial at a population level, even when vaccine stock is inadequate to vaccinate the entire population. Furthermore, ramping up the time ofthe COVID-19 vaccine rollout could help alleviate the effects of socioeconomic disparities, which are more perplexing to address in the short term, since wealth inequality is associated with vaccine inequity. The time of the initial COVID-19 vaccine rollout also significantly affected SARS-CoV-2 transmission and COVID-19 mortality, as determined by the SES-stratified mechanistic model.
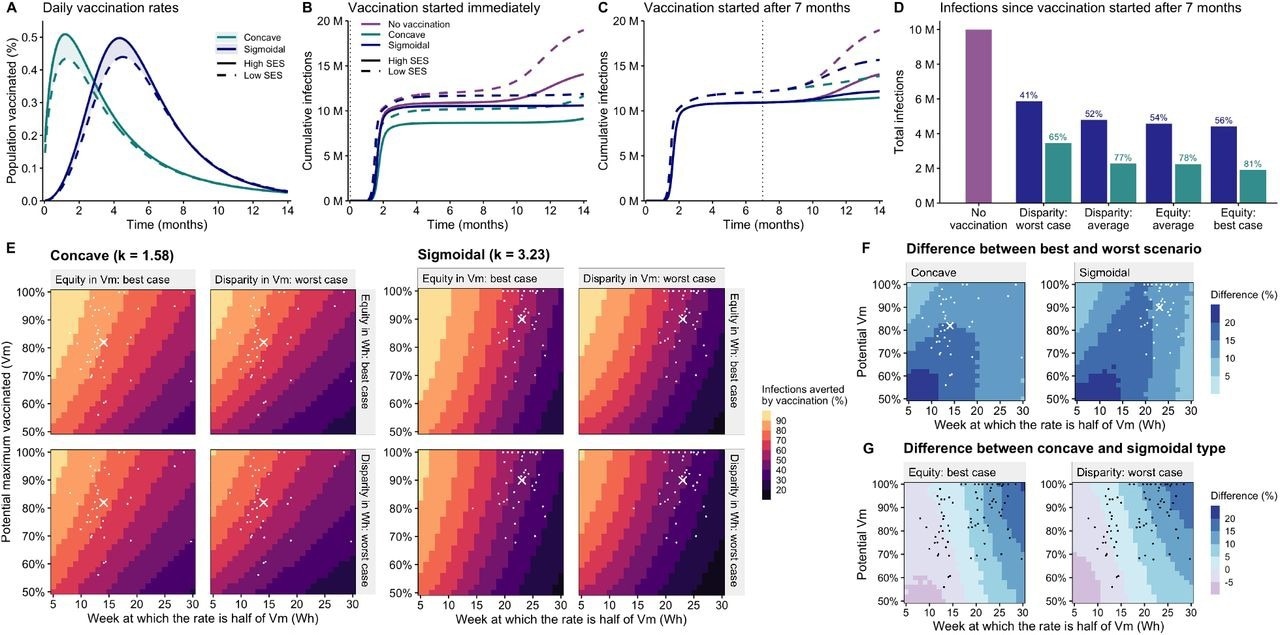
(A) Average daily vaccination rates for each type and SES group (per-country rates shown in fig. S13). In the sigmoidal type, the parameters for high SES are Vm = 89% and Wh = 23 weeks, while for low SES are Vm = 82.5% and Wh = 24 weeks. For both SES groups, k = 3.23, the average across SES. In the concave type, the parameters for high SES are Vm = 82.2% and Wh = 14 weeks,s while for low SES, they are Vm = 75.5% and Wh = 15 weeks. For both SES groups, k = 1.58. (B) Cumulative cases per 10,000 with vaccination starting immediately. (C) Cumulative cases per 10,000 with vaccination starting at t = 7 months. (D) Cumulative cases per 10,000 after 14 months under 4 scenarios of socioeconomic disparity: disparity: average, disparity: worst case (95th percentile), equity: average (averaging high SES and low SES parameters), and equity: best case (assuming vaccination of the low SES group follow the same parameters as the high SES group. (E) Cases averted by vaccination. Keeping k = 1.58 for concave and k = 3.23 for sigmoidal, we fixed the low SES parameters at a constant disparity from high SES based on the 95th percentiles of the observed data (ΔVm = 21%, ΔWh = 6 weeks), or considered low SES parameters equal to high SES (equity). The effect of varying parameter k can be found in figure S17. (F) The difference in cases averted under the best-case equity scenario and worst-case disparity for both concave and sigmoidal types. (G) The difference in cases averted under concave versus sigmoidal types for both best-case equity and worst-case disparity. Average high SES parameters are illustrated with a cross, while country-specific parameters for high SES are shown with dots.
Conclusions
The current study extensively analyzed the temporal trends of COVID-19 vaccination from multiple countries across five continents. To this end, COVID-19 vaccine inequity was found to exist within and between countries, which impacted disease burden and mortality.
While it remains crucial to address socioeconomic disparities, a better solution for the short term could be modifying the speed of vaccine rollout, as this appears to be unrelated to socioeconomic metrics. Therefore, promoting faster initial vaccine uptake could potentially reduce or minimize the effects of inequitable vaccination on the incidence of COVID-19 and subsequent deaths for all, irrespective of their socioeconomic status.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.