The gut microbiota developed after birth plays a significant role in shaping the immune system's maturation and impacting infants' susceptibility to allergic reactions. The gut microbiota of infants develops gradually and sequentially during the first years of life.
Breastfeeding has the highest impact on gut microbiota development. Mother's milk is the best natural source of many beneficial bacteria, including Bifidobacterium sp., Lactobacillus sp., and Staphylococcus sp.
In contrast, infant formulas cause relatively faster maturation and early diversification of the gut microbiota, leading to an enrichment of anaerobic bacteria and a reduction of beneficial bacteria.
Dairy companies are now focusing on preparing infant formulas as close as mother's milk to ensure proper development of the gut microbiota and induction of robust immunity in infants.
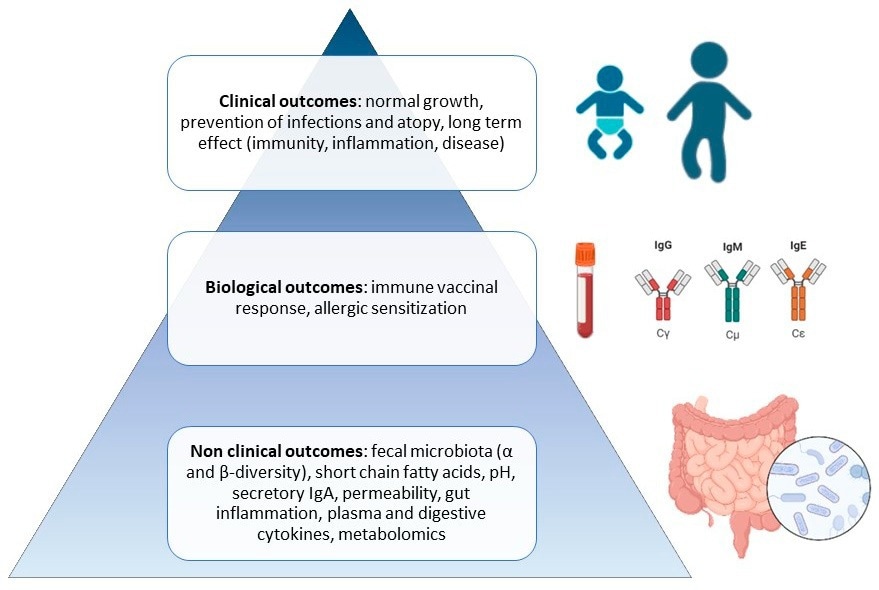
Pyramid of preclinical and clinical expected outcomes of pre-, pro-, syn-, and postbiotics during infancy.
Impact of probiotics
Probiotics are live microorganisms with acceptable safety and health benefits. These microorganisms are generally isolated from the human gut or traditional fermented foods.
Infant formulas supplemented with B. lactis Bb-12 (probiotic Bifidobacterium) are known to have immune-modulatory properties. B. lactis Bb-12-supplemented infant formulas also stimulate the production of secretory immunoglobulin A (IgA) to provide protection against pathogens and toxins and reduce the risk of respiratory infections and asthma for up to 5.5 years of age.
Infant formulas supplemented with Lactobacillus F19 have been found to increase the production of interleukin 2 (IL-2), IL-4, and IL-17A compared to that caused by breast milk. These pro-inflammatory cytokines are essential for host defense against pathogens.
Infant formulas supplemented with Lactobacillus reuteri DSM 17938 have been found to increase the proportion of beneficial bacteria and reduce the proportion of detrimental bacteria in infants.
Infant formulas supplemented with Lactobacillus rhamnosus GG (LGG) have been found to reduce gut inflammation in infants who are allergic to cow milk proteins. Formulas supplemented with Bifidobacterium animalis sp. lactis HN019 have been shown to reduce the risk of infection in infants.
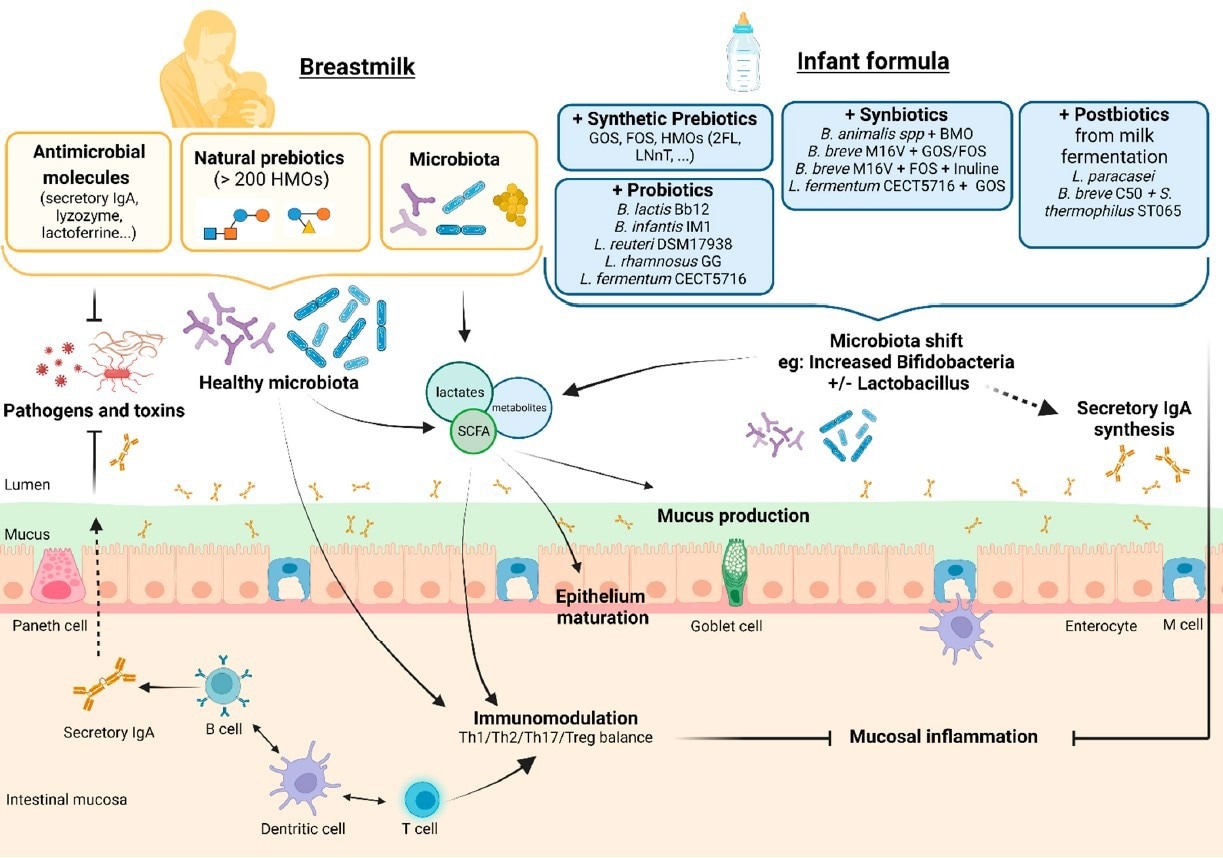
Supposed effects on the intestinal barrier, immunity, and microbiota of infant formula supplemented with pre-, pro-, syn-, and postbiotics compared to breastfeeding. Legend: BMOs— bovine-milk-derived oligosaccharides; FOSs—fructo-oligosaccharides; GOSs—galacto-oligosaccharides; HMOs—human milk oligosaccharides.
Impact of prebiotics
Prebiotics are present in many fiber-rich foods. Although humans cannot digest prebiotics, host microorganisms can metabolize them to provide various health benefits. Prebiotics selectively stimulate specific bacteria and, thus, induce the production of beneficial short-chain fatty acids.
Human milk oligosaccharide is a highly prevalent prebiotic in breast milk. Infant formulas supplemented with synthetic human milk oligosaccharides have been shown to induce the proportion of beneficial bacteria and reduce the adhesion of pathogens to epithelial cells.
Infant formulas supplemented with galacto-oligosaccharides (another prebiotic) have been shown to reduce inflammation, stimulate intestinal barrier function, reduce gastrointestinal colonization of Clostridium, and reduce the risk of respiratory tract infections. Infant formulas supplemented with fructo-oligosaccharides have been found to have similar benefits.
Infant formulas supplanted with both galacto-oligosaccharides and fructo-oligosaccharides at a ratio of 9:1 have been found to reduce the rate of atopic dermatitis, upper respiratory tract infection, fever, and antibiotic use in infants.
Impact of synbiotics
Synbiotics are a mixture of live microorganisms and substrates utilized by host microorganisms to provide health benefits.
Infant formulas supplemented with Bifidobacterium breve M-16V and oligosaccharides have been found to reduce the number of asthma symptoms, risk of atopic dermatitis, rate of antibiotic and anti-asthmatic medicine use, and frequency of infection-related hospitalization.
Infant formulas supplemented with L. fermentum CECT5716 and galacto-oligosaccharides have been found to reduce the risk of gastrointestinal and respiratory infections.
Impact of postbiotics
Postbiotics are a mixture of non-living microorganisms and their components with health benefits.
Infant formulas supplemented with Bifidobacterium breve C50, and Streptococcus thermophilus ST065 (lactic acid-producing bacteria) have been found to reduce the severity of gastrointestinal, respiratory, and dermal infections. These preparations are also beneficial for infants allergic to cow milk proteins.
Infant formulas supplemented with Bifidobacterium animalis sp. lactis CECT 8145 BPL1TM (thermally inactivated postbiotic) have been found to reduce the episodes of dermatitis, bronchitis, and bronchiolitis.