When cells cannot access glucose as an energy source, the body turns to alternative fuels, such as fat. This process produces substances known as ketones, which can accumulate in blood and urine. In this interview, News-Medical spoke with Marcin Pacek about the importance of ketone measurements and about how, why, and when to take measurements.
Could you introduce yourself and provide us with an overview of what ketones are?
My name is Marcin Pacek, and I am the Senior Director of Medical and Scientific Affairs in Europe at Nova Biomedical.
Ketones are substances that the body makes if cells do not get enough glucose, the body's primary energy source. Ketones can be detected in blood or urine, and high ketone levels might indicate ketoacidosis. In the case of diabetic patients, diabetic ketoacidosis (DKA) is a severe complication of diabetes that can lead to a coma or even death. It is a condition more common in type 1 diabetes, particularly soon after diagnosis, but it can also occur in type 2 diabetics, and in patients taking certain medications known as SGLT2 inhibitors.
Are there different types of ketones?
Yes, there are 3 different ketones found in humans. Beta-hydroxybutyrate (BHB) accounts for the majority, at more than 80% of total ketones. The other two ketones, acetoacetate (AA) and acetone account for the rest.
The physiology of ketone production is complex but basically starts with AA, which is made when fatty acids are broken down. Acetoacetate gets quickly converted to BHB in the mitochondria, predominantly in the liver, and BHB can be used by the body as an alternate energy source. Acetone is produced by spontaneous decarboxylation of AA, and is excreted partially by the lungs, which gives the breath a characteristic sweet odor.
How does the body use ketones, and what is their function?
Ketone body metabolism includes ketone body synthesis, known as ketogenesis, and breakdown, or ketolysis. When the body goes from a fed to a fasted state, the liver switches from carbohydrate utilization and fatty acid synthesis to fatty acid oxidation and ketone body production.
This metabolic switch is amplified in poorly controlled diabetes. In this state, energy is derived from fat, the ketone bodies generated in the liver enter the bloodstream, and they are used by other organs such as the brain, heart, kidney, and skeletal muscle. Ketone bodies are essential to maintain brain function in the absence of glucose, which has no other substantial non-glucose-derived energy source.
An increased concentration of ketone bodies in the bloodstream is known as ketonemia. Ketonemia is defined as a high concentration of ketone bodies in the blood during hunger, diabetes, fever, following surgery, being on a low carbohydrate diet, or after prolonged vomiting. Put simply, ketonemia is a result of increased blood concentration of ketone bodies caused by increased ketogenesis or impaired ketolysis.
What are the risks of an increase in the concentration of ketones in the body?
The increased concentration of ketones in the bloodstream, ketonemia, may lead to ketoacidosis. An especially dangerous case of ketoacidosis is diabetic ketoacidosis (DKA), which happens when diabetic patients are insulin deficient.
Diabetics treated with SGLT2 inhibitor therapy can also suffer from DKA without being insulin deficient. Non-diabetics can also experience ketoacidosis from alcohol or due to genetic or metabolic causes such as Succinyl-CoA:3-oxoacid CoA transferase (SCOT) deficiency. Ketoacidosis can lead to a ketoacidotic coma with potentially fatal outcomes if untreated.
Could you elaborate on diabetic ketoacidosis and the precise role ketones play in the development of this condition?
Diabetic ketoacidosis is a severe complication of diabetes that occurs when the body starts to overproduce ketones.
Diabetic ketoacidosis develops when the body does not have enough insulin to allow glucose to enter the cells. As a result, the body begins to use fat as its fuel, breaking it down instead of glucose. This process produces a build-up of ketones in the bloodstream, eventually leading to diabetic ketoacidosis if unchecked.
DKA is often triggered by illness, infection, or a problem with insulin therapy. Patients with Type I diabetes or those that frequently miss insulin doses have the highest possibility of developing diabetic ketoacidosis.
An infection or other type of illness can cause the body to produce a higher level of certain hormones such as adrenaline or cortisol. These hormones counter the effect of insulin, sometimes triggering an episode of diabetic ketoacidosis.
Typical infections that can lead to DKA are pneumonia and urinary tract infections, as these are common. Many times diabetic patients with gastroenteritis decrease their insulin dose because they are not eating much, and this can also be a trigger. Poorly compliant patients who frequently miss insulin doses or those who have inadequate insulin therapy can develop diabetic ketoacidosis.
How exactly can ketones be measured?
Ketone bodies can be measured in a central lab or using point-of-care meters.
Point-of-care meters, such as the Nova StatStrip and Nova Max Plus blood glucose and ketone meters use strip-based technology to detect BHB in whole blood. These meters enable self-testing of ketones by people with diabetes, testing by caregivers in clinics, schools, ambulances, and at the bedside, which allows for early detection or prevention of DKA.
The method used most widely in the central lab measures B-Hydroxybutyrate dehydrogenase levels photometrically.
Other ketones can be measured semi-quantitatively using urine dip sticks.
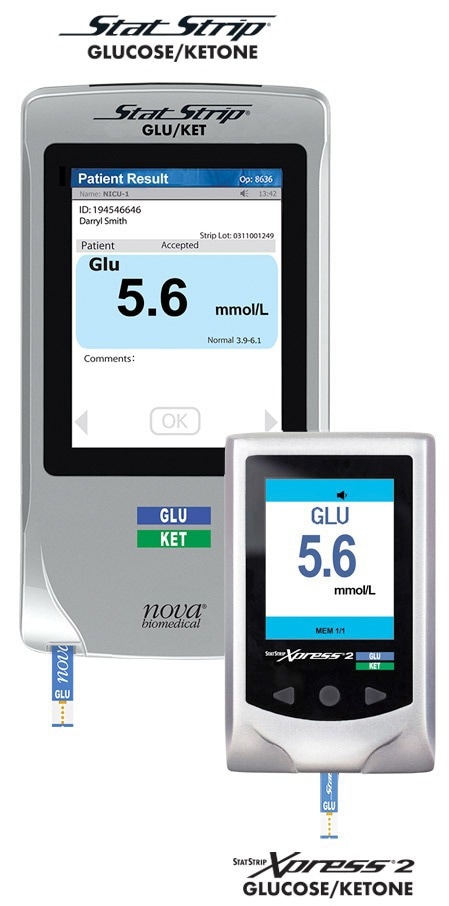
Image Credit: StatStrip Glucose/Ketone meter / Nova Biomedical
What is the most effective way to measure ketone levels in the body?
It is essential to measure ketones when glucose levels are high in diabetic patients. Ketone measurement is essential in DKA.
It may also be necessary to measure ketones in other conditions, such as glycogen storage disease (GSD), or in those following a ketogenic diet, which is widely used to treat epileptic patients. The primary focus of ketone measurement, however, is in diabetic patients to avoid DKA.
Measuring ketone levels in the blood typically involves measuring BHB only, whereas urine measurement measures acetone and AA. Urine measurement can be misleading in DKA because BHB levels can decrease but acetone levels may remain persistently high for several days, thus giving a picture of persistent DKA when the patient is out of danger. Thus, patients with DKA should only have ketones measured in the blood.
How do the guidelines and recommended standards help when it comes to measuring ketones?
Various clinical guidelines contain recommendations regarding ketone testing. The medical guidelines from the American Diabetic Association, Diabetes UK, and the European Society for Pediatric Endocrinology agree that glucose typically greater than 250 mg per deciliter combined with elevated blood ketones indicate probable DKA.
According to the guidelines, indications for ketone testing in the hospital include all cases of hyperglycemia where glucose levels are above 250 mg per deciliter in combination with an acute clinical condition such as emergency, post-operative period, intensive care, significant dehydration, or anuria.
Additionally, they include all cases of hyperglycemia when a diabetic patient is hospitalized, during acute illness or stress, or when blood glucose levels are consistently elevated.
The International Society for Pediatric and Adolescent Diabetes (ISPAD) advocates the use of capillary blood ketone testing methods that quantifies BHB for diagnosis and monitoring treatment of DKA.
Adopting these guidelines will significantly increase whole-blood ketone testing in hospitals and could result in more combined glucose and ketone diagnostic approaches for patient management.
What are the main benefits of detecting increased ketone levels early on?
Early diagnosis and treatment of a patient with DKA are essential to avoid significant morbidity and mortality. In a paper published in 2008, Sheikh et al. stated that measuring BHB allows for rapid diagnosis of DKA or redirection of diagnosis among acidotic patients presenting to the ED.
In 2007, Charles et al. stated that blood ketone measurement is a useful tool that allows clinicians to distinguish between simple hyperglycemia and potentially life-threatening ketotic states immediately. In 2006, Nannheim et al. stated that the point-of-care test for BHB is more valuable than glucose alone for diagnosing DKA and offers an immediate diagnosis of patients at triage.
The Joint British Diabetes Society recommends using whole blood BHB testing for diagnosing and monitoring the treatment of DKA. They also advise that patient management is based on reducing blood ketone levels in conjunction with other established parameters, meaning monitoring and measuring ketones in blood over time.
What measurement methods work best for ketone analysis?
In the guidelines for the management of diabetic ketoacidosis written by the British Society of Pediatric and Endocrinology and Diabetes, the authors recommend using capillary blood ketone measurements during treatment and blood ketone measurements if pH is not improving.
Blood ketone testing, rather than urine ketone testing, also improves outcomes in DKA, especially in the ICU/PICU wards. As published in 2007 by Noyes et al., DKA patients monitored by measurements of blood BHB had shorter ICU stays than patients monitored with urine ketones. That represents a cost saving of almost 30% for lab tests and a 70% reduction in clinical assessment.
Similarly, in a paper published in 2000 by Vanelli et al., DKA patients monitored by blood ketones reached the endpoint for intravenous therapy after 17 hours versus 28 hours for patients monitored by urine ketone testing.

Image Credit: Nova Biomedical
What are the differences between blood ketone measurements and urine measurements?
In urine, contrary to blood measurements, ketones may be present for several hours before the sample is collected and the testing performed, as urine can be in the bladder for some time. Therefore, testing for urine ketones is historic rather than real-time monitoring. Urine testing primarily measures acetoacetate and acetone, not BHB, which is the primary cause of ketoacidosis and therefore is the best ketone to monitor. As noted above, acetone can linger in the urine for up to several days after DKA has resolved, thus not providing a clear picture.
Additionally, DKA patients are often dehydrated and unable to provide urine samples. Severe DKA patients might be unconscious and, therefore, unable to urinate. The American Diabetes Association recommends that urine ketones not be used to diagnose or monitor the treatment of DKA. They recommend whole blood testing for BHB.
Urine test strips are easy to misinterpret since, over time, exposure to air results in incorrect readings. Urine test strips also typically have a short shelf life, so users must be careful to avoid expired strips.
Urine testing has many interferences that may give false positives, including nitroprusside, a common agent used for blood pressure management.
Urine measurement can be done in the lab or in a point of care (POC) format, and it is always semi-quantitative. Most importantly, it measures acetoacetate and acetone, not BHB. Beta-hydroxybutyrate represents over 80% of the total ketones, and providers can measure BHB in serum/plasma in a central lab, or the whole blood as a point-of-care test.
Would you say that blood testing for Beta-Hydroxybutyrate offers the best overview of a patient’s condition?
Many papers talk about the importance of ketone measurements, specifically BHB. In a paper by Rewers et al. from 2006, the author stated clearly that BHB testing is faster and more sensitive than urine ketone testing for detecting DKA.
In the paper published in 2008 by Sheikh-Ali et al., the authors stated that BHB permits the rapid diagnosis or exclusion of DKA among acidotic patients presenting to the ED. Additionally, Wallace et al. stated that the rate of fall of BHB in DKA could be used as an indicator of the adequacy of treatment.
Ketone testing is also useful in outpatient centers and diabetic clinics. It provides a simple patient monitoring tool for blood ketones during sick day visits.
It also provides rapid identification of developing ketosis and may prevent hospitalization through the simple verification of a patient's ketone and glucose levels after insulin pump failures or in a non-compliant patient. It is also a better alternative and more accurate than urine ketone strips.
Are there any other key benefits to measuring ketone levels in diabetic patients?
In a recent publication, a case study related to diabetic patients infected with COVID-19, the authors highlight that viral infections can lead to so-called acute diabetes. Diabetes is the most common comorbidity in COVID-19 patients, and that includes Type I and Type II diabetes.
Over 30% of diabetic patients died when they were infected with COVID-19. Diabetic patients that are COVID-19 positive have a significantly increased risk for severe outcomes and show the highest risk of DKA development.
In the study, diabetic patients with high levels of HbA1c (over 12) and very low pH (below 7.05) also had extremely high levels of ketones (above 4.5). Unfortunately, most of them died, leading to the conclusion that diabetic patients had a significantly increased risk of DKA when combined with COVID-19 infection. There is a high mortality rate, especially under ventilation, and tight glycemic control must be a priority.
SGLT2 inhibitors (empagliflozin, canagliflozin, dapagliflozin) are a newer class of antidiabetic drugs that are being more widely used, particularly in type 2 diabetics. There have been reports of an increased incidence of DKA with normal blood sugars (euglycemic DKA) in patients on these medications, due to their effects on the insulin to glucagon ratio, and their effectiveness in lowering blood sugar. Thus in this patient group, which will be increasing over time, ketone measurement even in the setting of a normal blood sugar is important if a patient is unwell.
Would early detection of DKA improve the clinical outcome for COVID-19 patients?
In a retrospective study on COVID-19 patients gathered from three hospitals in North London, almost 64% developed DKA. Eighty percent of them had Type II diabetes. All of them had a high ketone concentration with a median of 6 mmol/L. Both intensive care admission and mortality rate were significantly higher in the DKA group.
Surprisingly, 27 out of 42 non-diabetic patients developed ketosis, suggesting that COVID-19 infection may somehow trigger non-diabetic DKA events. When comparing those two groups, the diabetic patients who developed ketosis had a significantly prolonged hospital stay of 33 days versus 17 days and a significantly increased mortality rate of over 30% versus 4%.
Therefore, early diagnosis and treatment of DKA are essential in managing COVID-19 and reducing morbidity and mortality. It is estimated that 50% of hospital admission for DKA could be prevented with improved outpatient treatment and self-care.
About Dr. Pacek
Marcin Pacek joined Nova Biomedical in December 2018, as the EU Senior Director, Medical and Scientific Affairs. Marcin holds a Ph.D. in Biology and an MBA. His career evolved from scientist to higher management with growing experience in Healthcare, Medical Devices and POC diagnostics. He’s an expert with hands on knowledge in IVD, laboratory techniques and automatization, biomarkers, with emphasis on blood coagulation and anticoagulants. As a Senior Director at Nova Biomedical, Marcin is responsible for Medical and Scientific operations in Europe, Middle East and Africa, coordinating the work of the Medical and Scientific team in each country.
About Nova Biomedical
Nova Biomedical develops, manufactures, and sells advanced technology blood testing analyzers. We employ over 1,200 people, with sales and service subsidiaries in eight countries and distributors in more than 91 additional countries.
Nova has manufacturing facilities in Waltham and Billerica, Massachusetts; and Taipei, Taiwan. Nova is one of the 25 largest in vitro diagnostic companies in the world and the largest privately owned in vitro diagnostic company in the United States.