Over the last decade, scientists have explored the association between gut microbiota and the brain and affected neurologic manifestations. These studies have indicated that gut microbiota influences neurogenesis, behavior, emotions, cognitive development, and the progression of neuropsychiatric diseases. A new study published in the journal Frontiers in Medicine reviewed recent literature on the link between gut microbiota, the brain, and neurological disorders.
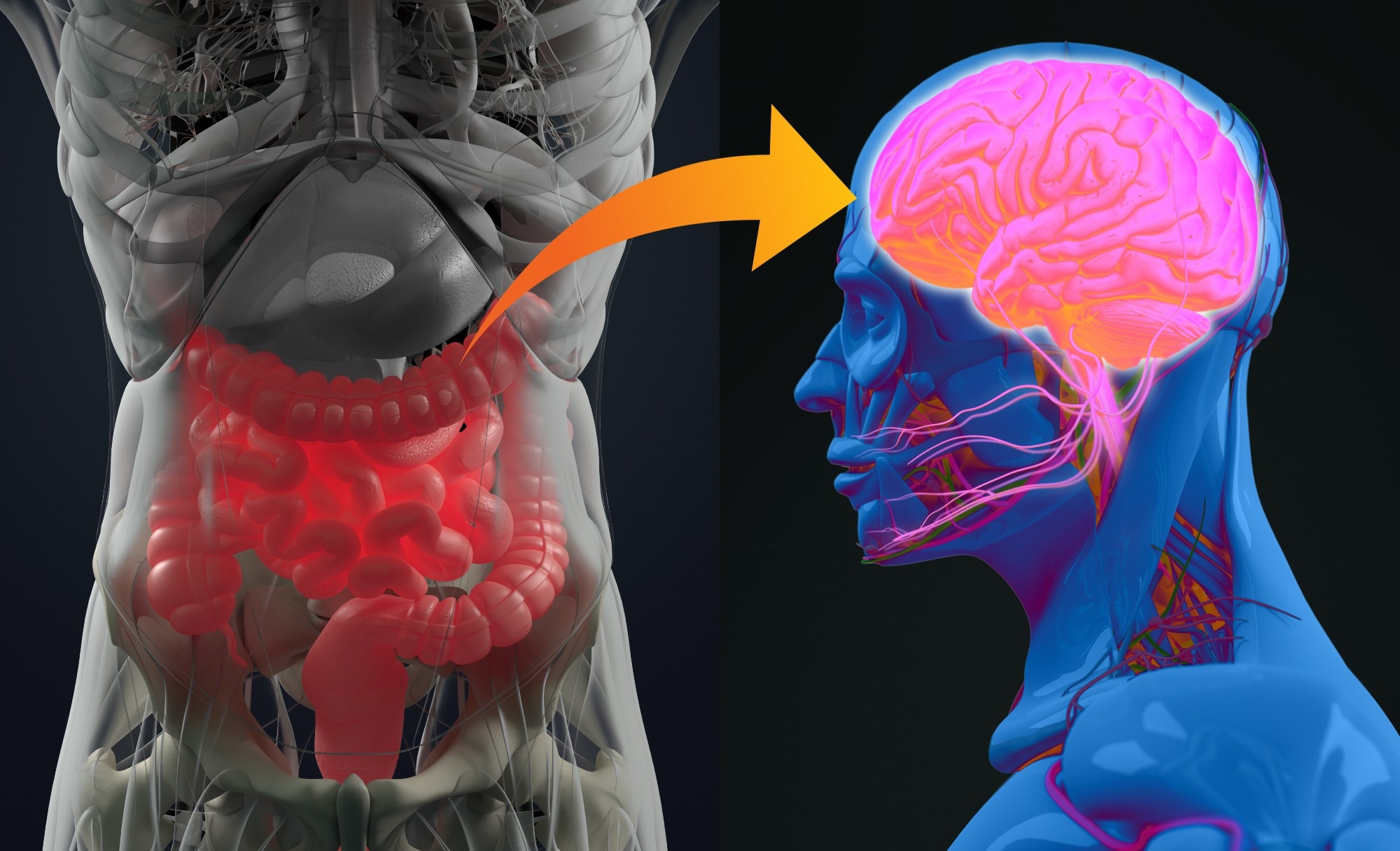 Review: Guts Imbalance Imbalances the Brain: A Review of Gut Microbiota Association With Neurological and Psychiatric Disorders. Image Credit: Anatomy Image / Shutterstock
Review: Guts Imbalance Imbalances the Brain: A Review of Gut Microbiota Association With Neurological and Psychiatric Disorders. Image Credit: Anatomy Image / Shutterstock
Relationship Between Gut Microbiota and Brain Manifestations
Gut microbiota can modulate and influence immune system functioning, cerebral activity, metabolic and nutritional homeostasis, and intestinal barrier integrity. Thereby impacting the physiological functions of the host. It has been observed that microbes are key signaling components in bidirectional communication of the gut-brain axis.
Disturbances in the brain-gut axis cause gastrointestinal symptoms, such as functional biliary pain, gastroesophageal reflux disease (GRD), cyclic vomiting syndrome (CVS), gastroparesis, and chronic abdominal pain. Prior research revealed that these disorders affect the neurenteric system.
Scientists have focused on the incidence of neuropsychiatric effects of gut microbiota. Several studies have indicated that gut dysbiosis influences neurological conditions such as anxiety, depression, Alzheimer’s disease, multiple sclerosis, schizophrenia, Parkinson’s disease, bipolar disorders, epilepsy, and dementia.
Diet influences gut microbial population. For instance, an animal-based diet increases the abundance of Alistipes, Bilophila, and Bacteroides and reduces the levels of Firmicutes. These imbalances affect digestion and other physiological functions. Firmicutes are associated with the effective metabolization of dietary plant polysaccharides; hence, lowering their abundance is expected to affect digestion adversely.
Gut microbiota biosynthesizes neurotransmitters, interacts with the central nervous system (CNS), and affects neurological health status. Hence, gut dysbiosis leads to the incidence of neurodegenerative illnesses.
Commercially available antidepressants contain antimicrobial properties against particular microbes of the human gut, such as Akkermansia muciniphila, Bifidobacterium animalis, and Bacteroides fragilis, which may exacerbate existing neurological illnesses. A prior study indicated that a small amount of Faecalibacterium in the gut is linked to depression.
Several studies have shown that the level of Bacteroides is significantly reduced in patients with major depressive disorder. Generalized anxiety disorder (GAD) is associated with negative thinking, irritability, sleep problems, and muscle tension. In addition, gastrointestinal tract inflammation is linked to gut dysbiosis that activates the release of pro-inflammatory cytokines and enhances tumor necrosis factor-alpha (TNF-α), directly related to anxiety manifestations.
It was observed that increased abundance in gut Bacteroides is related to anxiety-like disorders. In addition, low levels of Faecalibacterium, Lachnospira, Eubacterium, and Sutterella are found in patients with GAD.
Bipolar disorder (BD) is another neuropsychiatric disorder that is widely prevalent across the world. BD patients experience hyper manic or depressive conditions, where patients undergo periods of acute low mood, intense unhappiness, feelings of despair or high mood, extremely positive thinking, and low sleep requirement.
Gut microbiome imbalance has been linked to the incidence of BD. Several studies have indicated that patients with BD have increased bacterial translocation markers that originated from the intestinal lumen. In addition, BD is linked with obesity and metabolic disturbances, which enhances the risk of a worse disease prognosis.
A low level of Faecalibacterium has also been associated with BD. In addition, Clostridiaceae and Collinsella, which promote carbohydrate fermentation and generate short-chain fatty acids, were discovered to be important in maintaining gut barrier integrity. Notably, low levels of Bifidobacterium, due to cortisol production, adversely influenced stress response. Gut dysbiosis related to gastrointestinal inflammation was linked to schizophrenia.
Several studies have revealed that neurological disorders, including autism and schizophrenia, negatively affect gut microbes. Dementia is a psychological disorder that causes weak memory, changes in personality and thinking, and impairs reasoning. It was observed that fluctuations in Bacteroides levels directly affect the stimulating factors linked to cognitive decline in dementia. Notably, Lactobacillus and Bifidobacterium were found to improve the activity and release of neurotransmitters (acetylcholine), which affect learning and memory processes.
Probiotic Therapy for Neurological and Psychiatry-Associated Disorders
Recent studies have indicated that the host microbiome must be targeted to develop new psychotropic drugs for treating mental illnesses like depression. Several prebiotic and probiotic formulations have been developed to treat mental disorders.
Formulations directly affecting gut microbes and brain relationships are called “psychobiotics.” They provide anxiolytic and antidepressant effects that modify emotional, systemic, cognitive, and neural parameters.
Animal studies have indicated that probiotic strains, such as Lactobacillus rhamnosus, effectively decrease stress-related behavior and corticosterone release. Bifidobacterium breve is another probiotic strain used to treat psychiatric and gastrointestinal abnormalities in patients with major depressive disorder. Another study obtained favorable results in treating stressed rats with Lactobacillus fermentum PS150. This strain not only alleviated stressed symptoms but also lowered cognitive deficits.