In a recent study posted to the medRxiv* preprint server, researchers in France compared the efficacy of Pfizer-BioNTech original/BA.4-5 bivalent vaccine compared to messenger ribonucleic acid (mRNA) original (ancestral) monovalent vaccines against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
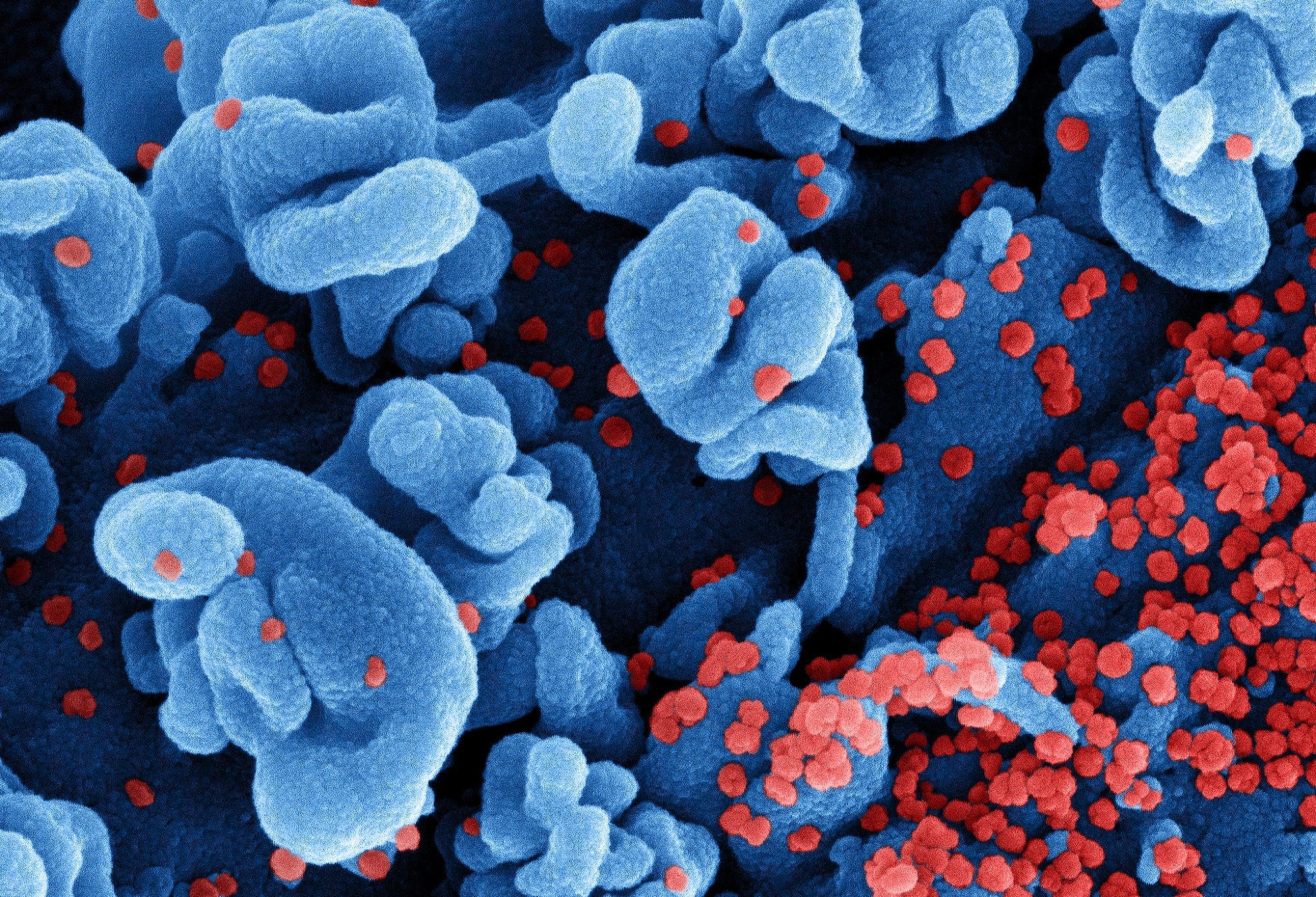 Study: Protection against symptomatic SARS-CoV-2 BA.5 infection conferred by the Pfizer-BioNTech Original/BA.4-5 bivalent vaccine compared to the mRNA Original (ancestral) monovalent vaccines – a matched cohort study in France. Image Credit: NIAID
Study: Protection against symptomatic SARS-CoV-2 BA.5 infection conferred by the Pfizer-BioNTech Original/BA.4-5 bivalent vaccine compared to the mRNA Original (ancestral) monovalent vaccines – a matched cohort study in France. Image Credit: NIAID

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Background
Due to the exceptional immune-evasion abilities of Omicron and its subvariants, the effectiveness of vaccines targeted at the ancestral SARS-CoV-2 strain dramatically worsened against Omicron infections.
Given the flexibility of the mRNA technology, researchers quickly developed a novel, next-generation coronavirus disease 2019 (COVID-19) vaccine for countering Omicron sublineages BA.1 and BA.4/5, referred to as bivalent vaccines. The French government introduced these vaccines for booster campaigns in early October 2022.
So far, all in vitro studies evaluating neutralizing antibody (nAb) titers induced by bivalent booster vaccines have concluded conflicting results. Hence, there is a shortage of data favoring their use over original monovalent vaccines. Moreover, studies performing these assessments in real-world settings have only compared people who had received a bivalent booster with those not boosted by any vaccine. Overall, data on the effectiveness of bivalent vaccines compared to monovalent vaccines is scarce or absent.
About the study
In the present study, researchers compared the extent to which Omicron BA.4-5 bivalent and monovalent vaccines conferred protection against symptomatic SARS-CoV-2 infection. In turn, they built a retrospective closed cohort comprising adults 60 years and older who received a booster dose between October 3 and November 6, 2022, per data from the French national surveillance databases.
Next, the researchers divided the study cohort into two matched groups; the first group received a booster dose of the monovalent COVID-19 vaccine, and the other received a bivalent vaccine. The cohort matching variables included the booster rank, boosting week, and the participant's residence.
The primary study outcome was the incidence of symptomatic COVID-19 on a reverse transcription-polymerase chain reaction (RT-PCR) test at least seven days after receipt of a booster dose. The study follow-up period was between October 2022 and March 2023. During the later study period, the dominant SARS-CoV-2 variants were BA.5 sublineages, e.g., BQ.1.1.
Study findings
The study cohort comprised 136,852 individuals, of which 85% had received a second booster dose. The average follow-up period was 77 days, during which the authors noted 1,147 SARS-CoV-2-positive test results among individuals who received a booster dose of an mRNA vaccine targeting the ancestral SARS-CoV-2 strain. The number of SARS-CoV-2-positive cases in individuals who received a booster dose of the bivalent vaccine was 1,025.
Though boosting by a bivalent vaccine conferred statistically significant additional protection of 8% against symptomatic SARS-CoV-2 infection compared to monovalent vaccines, it was still minimal. Furthermore, this protection also did not account for additional protection conferred by a recent prior infection by Omicron BA.2 or BA.4-5 subvariant, i.e., 8% vs. 74%.
In comparison, relatively older previous infections among boosted individuals (caused by variants more genetically distinct from the circulating strains) conferred lower immune protection. Notably, the analysis restricted to participants with no previous infection showed no marked difference.
Conclusions
The bivalent vaccine used in this study only partially compensated for Omicron and its subvariants' extraordinary immune evasion potential. However, more importantly, a recent receipt of a booster dose, irrespective of its type (a monovalent or a bivalent vaccine), conferred more protection against symptomatic COVID-19 than any former mRNA vaccine used for boosting. Thus, booster vaccination could maximize immunity against COVID-19, especially among high-risk populations.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.