For very long, researchers have hypothesized that lipopolysaccharide (LPS) endotoxins shed from the outer membrane of Gram-negative bacteria, e.g., gut-resident Bacteroides fragilis and Escherichia coli, contribute to the pathogenesis of Parkinson's disease (PD).
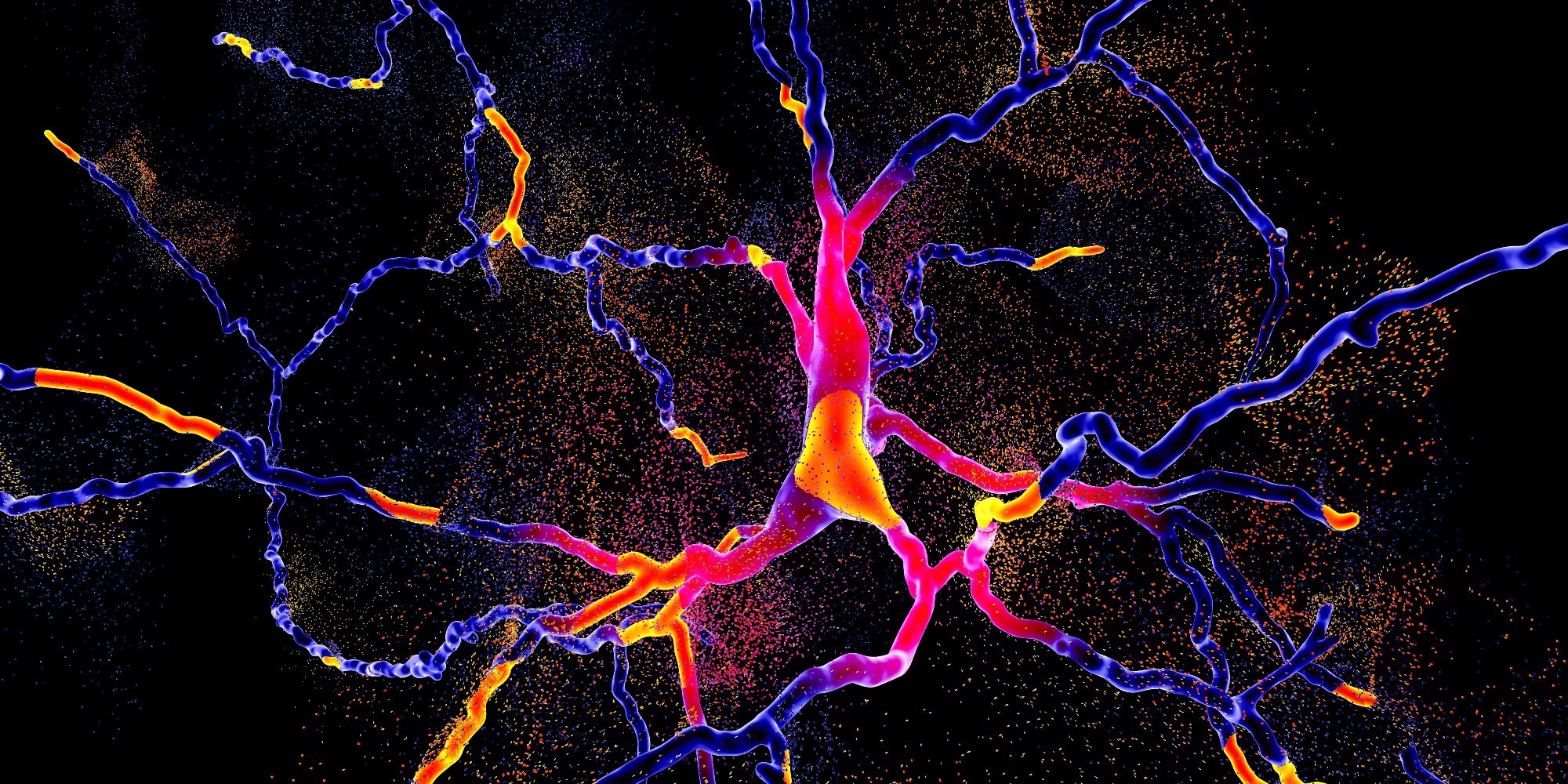 Study: The Endotoxin Hypothesis of Parkinson's Disease. Image Credit: Kateryna Kon / Shutterstock
Study: The Endotoxin Hypothesis of Parkinson's Disease. Image Credit: Kateryna Kon / Shutterstock
Background
Besides gut-resident bacteria, bacterial infections, such as periodontitis (gum disease), increases inflammatory LPS found in the blood and brain and PD risk. The diet also affects circulating LPS levels, especially high-fat meals that trigger metabolic endotoxemia.
However, the primary cause of increased LPS levels in the blood is increased gut permeability. In the gut, endotoxins are relatively benign; however, when translocated to the bloodstream, they promote α-synuclein aggregation to trigger systemic and brain inflammation that exacerbates neuronal loss.
Intriguingly, since PD is a biologically heterogeneous neurodegenerative disease, elevated LPS endotoxins in serum might be particularly relevant to disease pathogenesis in only a subgroup of PD patients. Accordingly, early gastrointestinal (GI) symptoms in PD are also not universal, with only ~30% of patients with new-onset PD reporting constipation.
About this study
In this study, about 25% of the PD patients had endotoxin levels higher than any of the controls; however, 70% of PD patients had normal levels of serum endotoxin. However, their sample set comprised just 41 PD patients and controls (small sample set). So, it would be interesting to monitor serum LPS levels of PD patients over days, months, and years and ascertain whether these elevate transiently or permanently concerning PD progression.
Next, the authors raised the technical challenges in LPS quantification using human blood samples. In this study, they used the Limulus amoebocyte lysate (LAL) assay and found an ~60% higher average LPS level in the serum of PD patients. This test quantifies the biological activity of LPS-containing samples in endotoxin units (EU) to induce blood coagulation of the horseshoe crab Limulus. Varying with LPS source, one EU roughly equates to 100 pg LPS.
However, since LPS blood concentrations are so low, most commercial assays fail to detect LPS. Also, the half-life of LPS in the blood is short. Thus, researchers emphasized using plasma (not serum) for LPS quantification in PD patients using collection tubes having low concentrations of heparin.
Further, the researchers highlighted that accidental exposure and injection of LPS into healthy humans could induce several non-motor symptoms observed among PD patients. The pathophysiological basis of PD is multifactorial, raising the possibility that the LPS-induced sickness symptoms are not unique. Experiments in mice have demonstrated that peripheral endotoxin increases blood–brain barrier (BBB) permeability and uptake of α-synuclein into the mice brains. This observation helped researchers arrive at a dual-hit hypothesis for PD: augmented levels of LPS endotoxin combined with aggregable α-synuclein drive the PD-related neuronal loss.
Secondly, the authors noted that microglia, brain macrophages mediating innate immunity and inflammation, become activated in the substantia nigra of PD patients. Even in healthy human volunteers, intravenous injection of LPS induced robust microglial activation in most brain areas within no time. During hypoxic conditions (and in the presence of interferon-gamma), LPS induced nitric oxide synthase (iNOS) in the glia to kill neurons.
Further, they identified the genetic basis of how LPS endotoxin activated the α-synuclein-expressing SNCA gene that triggered neuropathology. The endotoxin hypothesis, thus, might be relevant to both idiopathic and genetic forms of PD.
Conclusion
To conclude, if the endotoxin hypothesis holds, the researchers highlighted the need to evaluate many PD-targeted therapeutic strategies in clinical trials. First, therapies should manipulate the gut bacterial profile to reduce endotoxin-producing species and try reducing gut permeability. Techniques like fecal microbiota transplant (FMT) and non-steroidal anti-inflammatory drug (NSAID) use could help achieve these goals.
To protect animals from Gram-negative sepsis, they should be vaccinated only with detoxified LPS to induce anti-LPS antibodies. Drugs that reduce LPS receptor TLR4's expression and activity, e.g., Candesartan, could be a worthy intervention. Similarly, blocking complement receptor 3 and the P2Y6 receptor could hinder the microglial response to LPS.
Most importantly, trials testing multiple variants of the endotoxin hypothesis require patient selection according to their baseline endotoxin levels. Also, these studies should quantify LPS and its markers longitudinally in large PD and prodromal cohorts. Nonetheless, LPS endotoxin-related mechanisms appear highly relevant in a subset of PD patients.