A review article describing the utility of mRNA vaccines in disease prevention and treatment has recently been published in the journal Signal Transduction and Targeted Therapy.
Messenger RNA (mRNA)-based vaccines are developed using a single nucleotide sequence that acts as a template for protein (antigen) translation. These vaccines utilize the body’s endogenous machinery to translate and subsequently translocate fully functional proteins of interest to their suitable cellular locations to induce antigen-specific innate and adaptive immunity.
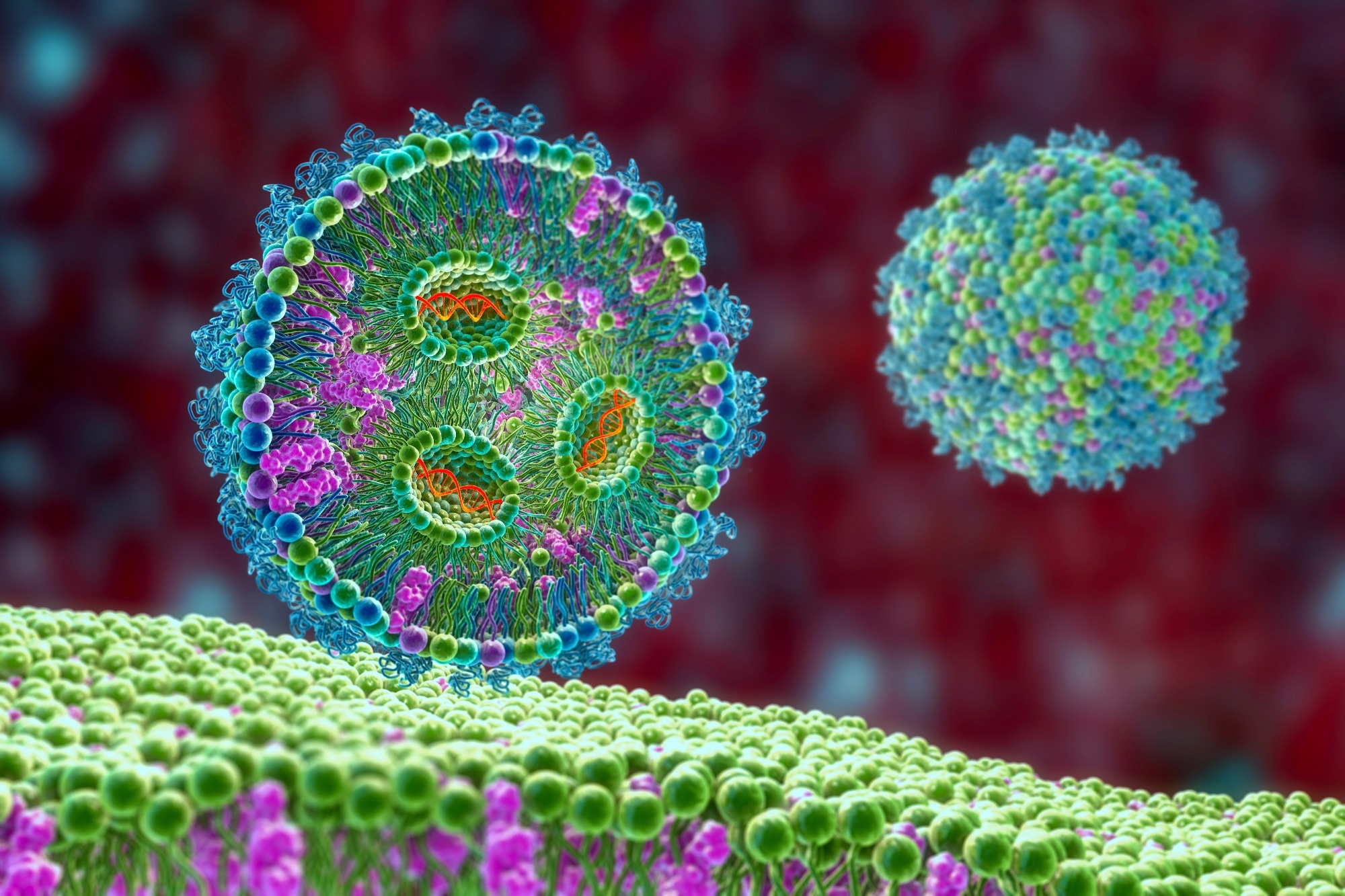 Review: mRNA vaccines in disease prevention and treatment. Image Credit: Kateryna Kon / Shutterstock
Review: mRNA vaccines in disease prevention and treatment. Image Credit: Kateryna Kon / Shutterstock
The mRNA vaccines are designed to encode any antigens based on the unique traits of diseases. Rapid and large-scale production of these vaccines through a cell-free process is possible because of the highly productive and cost-effective transcription reaction in vitro.
Two major disadvantages of mRNA vaccines include poor stability and high immunogenicity. However, advancement in vaccine design, development, and delivery technologies has made it possible to improve in vivo stability of mRNA vaccines, as well as to maintain a balance between the induction of strong vaccine-specific immune responses and irreversible adversities caused by persistent functions.
With the extraordinary performance in the recent coronavirus disease 2019 (COVID-19) pandemic, mRNA vaccines have emerged as a highly effective strategy in the prevention and treatment of many diseases, including infectious diseases, immunological diseases, cancers, and rare diseases.
mRNA vaccines in infectious diseases
The mRNA vaccines encoding pathogen-specific antigens are used to prevent many infectious diseases. In recent years, mRNA vaccines have shown tremendous potency in controlling the rapid spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative pathogen of COVID-19.
The spike glycoprotein present on the viral surface is the primary target for anti-COVID-19 mRNA vaccines because of its high immunogenicity and primary involvement in the viral entry process. Two mRNA vaccines encoding the spike protein have been developed to date. These vaccines are mRNA-1273, developed by Moderna, and BNT162b2, developed by BioNTech/Pfizer.
The mRNA-1273 is a lipid nanoparticle-encapsulated vaccine encoding the prefusion-stabilized full-length spike protein of SARS-CoV-2. The vaccine is capable of inducing strong humoral and cellular immune responses against the original SARS-CoV-2 and its D614G mutated variant. In clinical trials, two doses of this vaccine have shown 94% efficacy against SARS-CoV-2 infection and 100% efficacy against severe COVID-19. During the SARS-CoV-2 delta-dominated wave, about 88% vaccine efficacy has been observed against COVID-19 after 14 days or more of initial vaccination. The most commonly reported vaccine side effects are headache, chills, injection site pain, fatigue, and myalgia.
The BNT162b2 is also a lipid nanoparticle-encapsulated mRNA vaccine encoding prefusion-stabilized, membrane-anchored full-length spike protein of SARS-CoV-2. In clinical trials, two doses of this vaccine have shown 95% efficacy against SARS-CoV-2 infection. Three doses of this vaccine have shown equivalent efficacy against the original SARS-CoV-2 and its omicron variant. The most commonly reported side effects include injection site pain, fatigue, and headache.
Bivalent formulations of mRNA vaccines as a single booster dose have been approved by the US Food and Drug Administration (FDA) in August 2022. These formulations contain one viral component from the original (wild-type) SARS-CoV-2 and another from the omicron variant. These bivalent preparations have shown significantly higher efficacy than monovalent preparations against SARS-CoV-2 variants. Given the observed benefits, the FDA has approved only bivalent mRNA vaccines for further use as a single booster dose.
Several lipid nanoparticle-enclosed mRNA vaccines encoding membrane and envelop glycoproteins of the Zika virus have been developed and tested in animals. The findings indicate promising outcomes in terms of strong and durable humoral and cellular immune responses. However, further human trials are needed to explore vaccine efficacy.
The majority of mRNA vaccines developed against Human Immunodeficiency Virus (HIV) have failed to demonstrate any protective efficacy mainly because of the significant antigenic diversity of HIV envelope proteins and the dense glycan shield of the virus that hides vital epitopes. Recently, an mRNA vaccine concurrently expressing membrane-anchored HIV envelope and simian immunodeficiency virus Gag proteins has been developed. This vaccine has shown high efficacy in inducing neutralizing antibodies and T-cell response in monkeys.
The glycoprotein haemagglutinin on the surface of the influenza virus is the main target for developing mRNA vaccines against influenza. Several nucleoside-modified mRNA vaccines have been developed and tested in animals. These vaccines have shown promising and long-lasting efficacy against a number of influenza virus subtypes. Further human trials are needed to explore the safety and efficacy profiles of these vaccines.
The mRNA vaccines developed against human cytomegalovirus, respiratory syncytial virus, varicella-zoster virus, and rabies virus are still at their nascent stage of clinical investigation. More studies in animals as well as humans are needed to evaluate their safety and protective efficacy.
mRNA vaccines in cancers
The mRNA vaccines in cancers are mainly used as therapeutics instead of prophylactics. These vaccines are designed to encode tumor-associated antigens or neoantigens to induce anti-tumor immune responses. Many clinical trials are currently ongoing to test the therapeutic efficacy and safety of mRNA vaccines targeting many cancer types, including melanoma, brain cancer, non-small cell lung cancer, ovarian cancer, prostate cancer, blood cancer, digestive system cancer, and breast cancer.
Cancer is a highly heterogeneous and complex disease caused by genetic and epigenetic factors. This highlights the need for developing personalized mRNA vaccines to manage cancers. However, accurate detection and quantification of tumor neoantigens and the complexity of the tumor immune evasion process make it difficult to clinically apply personalized cancer mRNA vaccines. Moreover, immunosuppressive cells and regulators in the tumor microenvironment can suppress the T-cell response induced by these vaccines.
A combination therapy with anti-tumor monoclonal antibodies and personalized vaccines is believed to be effective for cancer management. Clinical trials investigating pembrolizumab in combination with neoantigen vaccination against melanoma or personalized vaccination together with temozolomide and radiotherapy against glioblastoma are currently ongoing.
mRNA vaccines in immunological diseases, tissue damage, and rare diseases
Many mRNA vaccines against autoimmune diseases, tissue damage, and rare diseases are still in the early stages of investigation. Sufficient information regarding the efficacies and challenges of mRNA vaccines against these diseases is unavailable.