Leukemia, characterized by unregulated clonal proliferation of hematopoietic stem cells, is the second leading cause of death in children. The role of the intestinal microbiota is closely linked to responses to therapies administered to leukemia patients.
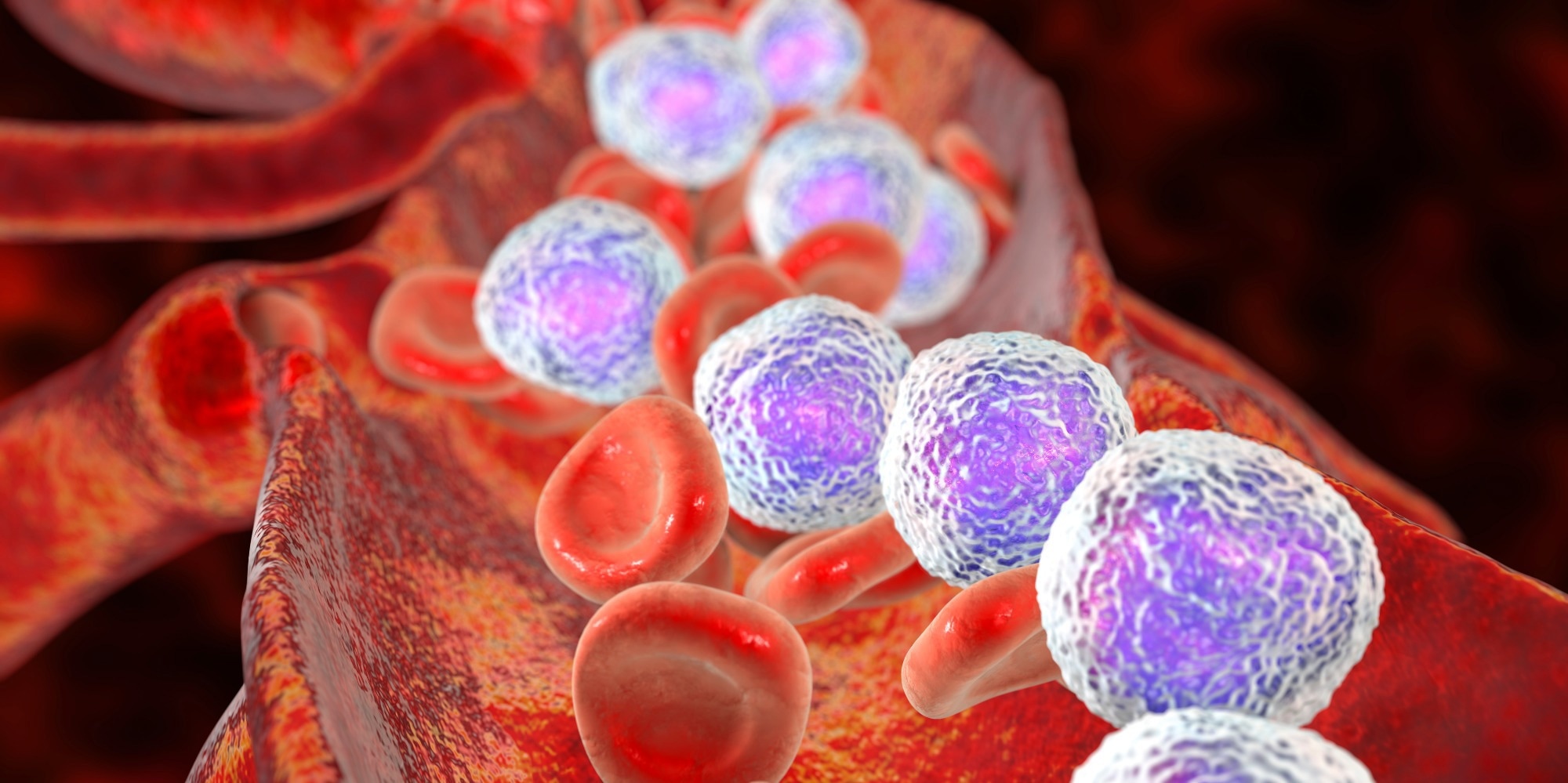 Study: Microbiota, Diet and Acute Leukemia: Tips and Tricks on their Possible Connections. Image Credit: Kateryna Kon / Shutterstock.com
Study: Microbiota, Diet and Acute Leukemia: Tips and Tricks on their Possible Connections. Image Credit: Kateryna Kon / Shutterstock.com
Diet and leukemia
Multiple dietary factors play crucial roles in human health through metabolism, immunological processes, and microbiota regulation. Previous studies have reported that maternal diet, alcohol consumption, and smoking during pregnancy increase the risk of leukemia in children.
An inverse association between maternal intake of fruits/vegetables and childhood acute lymphoblastic leukemia (ALL) has also been observed. Some studies indicate that the reduced childhood risk of ALL might be associated with higher maternal intake of fruits/vegetables and micronutrients such as folic acid, which is involved in DNA synthesis, repair, and epigenetic processes. Maternal malnutrition and reduced micronutrient levels could increase cortisol levels, thereby influencing fetal immune system development that may disrupt immune cell proliferation and organogenesis.
The risk of ALL in children increases when maternal diets include sugars and syrups with low levels of seafood, fish, beef, and beans. Recently, a systematic review highlighted the inverse association between a maternal diet rich in fruits/vegetables during pregnancy and ALL risk in children. To this end, the risk of ALL was positively associated with consuming more coffee or caffeinated beverages.
A higher consumption of caffeinated beverages and junk food among two to 12-year-old ALL or acute myeloid leukemia (AML) patients as compared to healthy controls has been reported. Furthermore, there is an inverse association between breastfeeding and childhood leukemia, with estimates suggesting that 14-19% of childhood leukemia cases could be prevented by breastfeeding for six months or more.
Childhood leukemia and maternal diet quality
Modulation of the gut microbiota by diet during pregnancy is of significant interest, given its potential contribution to maternal and infant health. Emerging evidence underscores the effects of specific nutrients on metabolic outcomes based on individual microbial patterns, suggesting the importance of personalizing nutrition therapies.
Gut microbiota changes occur during pregnancy, including reduced microbial richness and higher inter-individual diversity, with microbial patterns in late pregnancy similar to those in non-pregnant individuals with metabolic syndrome. Dysbiosis leads to metabolic abnormalities, such as increased gut permeability, abnormal production of short-chain fatty acids, and higher absorption of lipopolysaccharides.
Thus, maternal gut microbiota alterations could have implications for neonatal gut microbiota, as it is derived from the maternal gut. Reports suggest that cesarean section, intrapartum antibiotics, and infant formula use may disrupt microbiome development, thereby increasing the risks of infectious exposures and chronic inflammation in children and, possibly, ALL.
Leukemia drug pharmacokinetics and microbiota
The gut microbiota composition could influence the prognosis and complications of acute leukemia after chemotherapy or hematopoietic stem cell transplant. In particular, prebiotics/probiotics and dietary changes could reduce treatment-related side effects and enhance therapeutic efficacy. Chemotherapy drugs may also directly act on the microbiota or damage intestinal epithelium, causing dysbiosis, which could subsequently impact drug absorption and metabolism.
Epithelial barrier damage due to anti-tumor treatments may increase the abundance of specific bacteria, which could promote bacteremia and resistant bacterial infections. Methotrexate, often used to treat leukemia, can induce jejunal villi atrophy, increase goblet cells and inflammatory processes, and contribute to the collapse of muscularis mucosa. One study reported that the gut microbiota chemically modified the metabolism of various tested drugs.
Therapeutic strategies
Probiotics have been adopted to manage intestinal changes and treatment-related adverse effects. In one trial on ALL children receiving chemotherapy, oral probiotics reduced gastrointestinal complications, including flatulence, nausea, vomiting, and abdominal distension. In fact, prebiotic supplementation while undergoing chemotherapy may restore the microbiota, thereby alleviating therapy-related side effects.
Melatonin supplements have also been shown to augment gut microbiota diversity and composition and increase the abundance of Lactobacillus in mice. Thus, foods enriched with melatonin could help to modulate the gut microbiota after chemotherapy in leukemia patients.
Taken together, these findings indicate that an appropriate diet and prebiotics could be viable alternatives to support the management of microbiota alterations in leukemia.
Conclusions
Growing evidence highlights the role of the gut microbiota in modulating the effectiveness of leukemia treatment. Although many studies have investigated the microbiota as a targeted therapy for neoplastic diseases, there is limited data on the relevance of gut microbiota and dietary changes in leukemia. Therefore, further analyses are necessary to assess the relationship between leukemia, diet, and microbiota.
Journal reference:
- Furci, F., Cicero, N., Allegra, A., & Gangemi, S. (2023). Microbiota, Diet and Acute Leukemia: Tips and Tricks on their Possible Connections. Nutrients. doi:10.3390/nu15194253