Both are spatially intertwined in the cNTS, yet they do not overlap and respond to food intake with a delay, but show sustained activation.
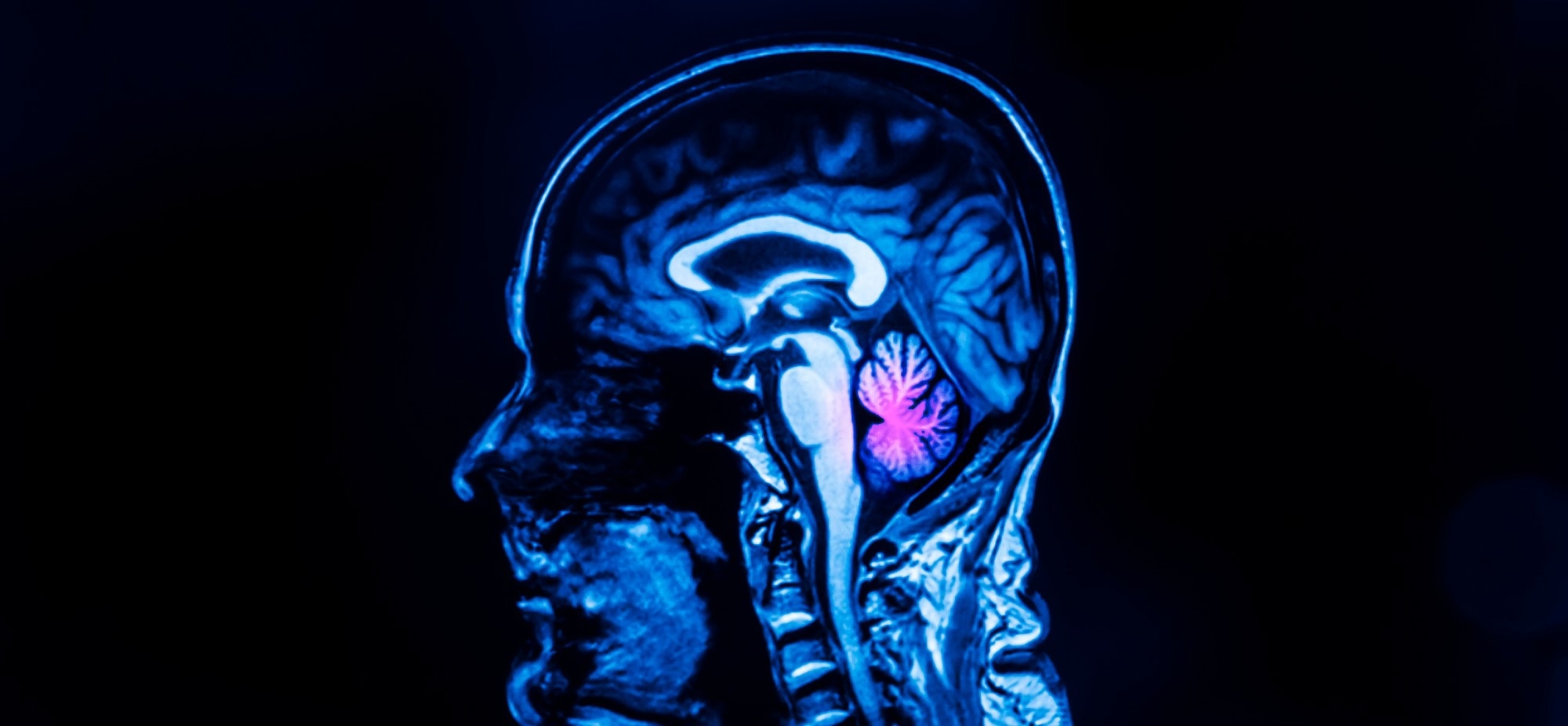 Study: Sequential appetite suppression by oral and visceral feedback to the brainstem. Image Credit: PeterPorrini/Shutterstock.com
Study: Sequential appetite suppression by oral and visceral feedback to the brainstem. Image Credit: PeterPorrini/Shutterstock.com
Background
The cNTS is the first site in the brain where almost all gastrointestinal (GI) signals transmitted by the vagus nerve are sensed and integrated.
In previous studies, researchers used anesthetized animals to understand the role of the cNTS in feeding behavior. These animals showed minimal specificity in their responses to GI stimuli.
However, the role of the cNTS in feeding behavior has not been tested in a conscious animal that generates sensory and motor feedback during food ingestion. This raises the possibility that cNTS neurons, like other sensory systems, show more functional specificity in awake animals.
Thus, there is a knowledge gap regarding the cNTS function when GI signals are slow (accumulating over minutes) during and after feeding, how it guides behavioral decisions, and whether it detects other ingestive cues regulating feeding behavior.
About the study
In the present study, researchers performed several experiments in Prlhcre knock-in mice to address queries redefining how the neuronal circuits that receive visceral feedback directly encode sensory signals generated during a meal.
First, they investigated how PRLH neurons express the fructooligosaccharides (FOS) gene in response to ingestion and how they inhibit feeding without inducing conditioned taste avoidance. Further, they made fiber photometry recordings of PRLH neurons in Prlhcre knock-in mice equipped with intragastric (i.g.) catheters while awake.
To test the hypothesis that GCG neurons track cumulative food intake on a timescale of minutes, the researchers controlled the rate at which mice were allowed to ingest Ensure (a liquid diet). Then, they measured the neural response of GCG neurons to different ingestion volumes and characterized their post-prandial activity in relation to the amount of food consumed.
Results
PRLH neurons in Prlhcre knock-in mice activated rapidly in response to the oral consumption of nutritive solutions but not through i.g. infusion. Moreover, their activation progressed differently during feeding trials using oral gavage versus i.g. infusion.
Optogenetic stimulation of PRLH neurons confirmed that these cells specifically regulated feeding, not water intake. Thus, infusion of 1.5 ml of the liquid diet 'Ensure' resulted in a ramping activation directly correlated with the amount infused, peaking minutes after infusion stopped (16±4 minutes), and remained elevated throughout the session.
The ramping activation remained similar in response to infusions of glucose and fat (Intralipid), with respective peaking times of 21±2 minutes and 22±4 minutes.
PRLH neurons remained activated for tens of minutes after nutrient infusion into the stomach, but this was considerably reduced during physiological (normal) feeding conditions. Indeed, time-locked responses to orosensory cues, including taste, dominated PRLH activity, suggesting a strong correlation with oral contact with food.
PRLH neurons tracked short-term orosensory cues, not the amount of food consumed. Further, taste was not necessary for their activation. However, PRLH neurons were more strongly activated by food than water, possibly due to varying sensory or behavioral properties.
GCG neuron activity was primarily driven by feedback from the stomach and intestines. Only food ingestion activated GCG neurons and inhibited its intake without inducing conditioned taste avoidance. GCG neurons tracked GI fill and remained activated from four to 10 minutes in response to cumulative food intake.
GCG neurons also showed a strong response to nutrient infusions. They were more sensitive to GI feedback and responded preferentially to GI stretch rather than gut peptides released in response to intestinal nutrients.
Continuous optogenetic stimulation of GCG neurons inhibited the consumption of solid and liquid food but not water. Importantly, these neurons did not control the dynamics of feeding, but their stimulation inhibited ongoing food consumption and reduced the initiation of ingestion bouts later.
Conclusions
PRLH neurons controlled feeding behavior on shorter timescales, whereas GCG neurons promoted post-prandial satiety on longer timescales.
In other words, negative feedback signals from the GI tract engaged two genetically distinct circuits in the cNTS, which controlled feeding behavior over short and long durations.
PRLH neurons limited the size of food ingestion bouts, thereby restraining the pace of food intake. They had little to no effect on total food intake. This response likely prevented the GI distress that occurs upon rapid food consumption.
Conversely, GCG neurons responded strongly to mechanosensory feedback from the GI tract, inhibiting ongoing food ingestion.
In the future, this might enable clinical use of glucagon-like peptide 1 (GLP-1) receptor agonists for sustained appetite reduction.