BFS and GFS are uncommon medical disorders that can lead to ethanol intoxication in individuals with poorly managed diabetes. The absence of alcoholic intoxication due to the bladder lumen's transitional epithelium distinguishes BFS. GFS patients can experience symptoms even without consuming alcohol due to alcoholic fermentation in the gut lumen. Yeast removal, antifungals or antibiotics, and changes to the underlying problems can treat both disorders. However, failing to recognize these factors might have grave legal implications.
In the present review, researchers examined the etiology, clinical characteristics, and diagnostic techniques of BFS and compared them to GFS.
 Gut and bladder fermentation syndromes: a narrative review. Image Credit: Magic mine / Shutterstock
Gut and bladder fermentation syndromes: a narrative review. Image Credit: Magic mine / Shutterstock
BFS: Introduction, pathophysiology, diagnosis, and treatment
BFS is a syndrome characterized by ethanol production in the urinary bladder of individuals with poorly managed diabetes. The first clinical occurrence of BFS occurred in 2020, and the patient failed abstinence monitoring. In 2020, researchers published the first experimentally proven example of ethanol fermentation in the bladder with ethanol produced by Candida glabrata. In BFS, the lack of alcoholic intoxication is critical since the bladder lumen comprises transitional epithelium with limited ethanol permeability.
Funguria is the presence of yeast, mainly Candida species, in urine due to yeast colonization in the bladder or widespread candidiasis. Funguria is frequent among older hospitalized patients, and Candida albicans is the predominant etiological organism. Alcoholic fermentation is a metabolic process occurring after glycolysis, allowing yeast species to replenish nicotinamide adenine dinucleotide (NAD) in anaerobic conditions. In cases of oxygen insufficiency for energy synthesis, crabtree-positive yeast, such as C. glabrata, initiate glycolysis or alcoholic fermentation.
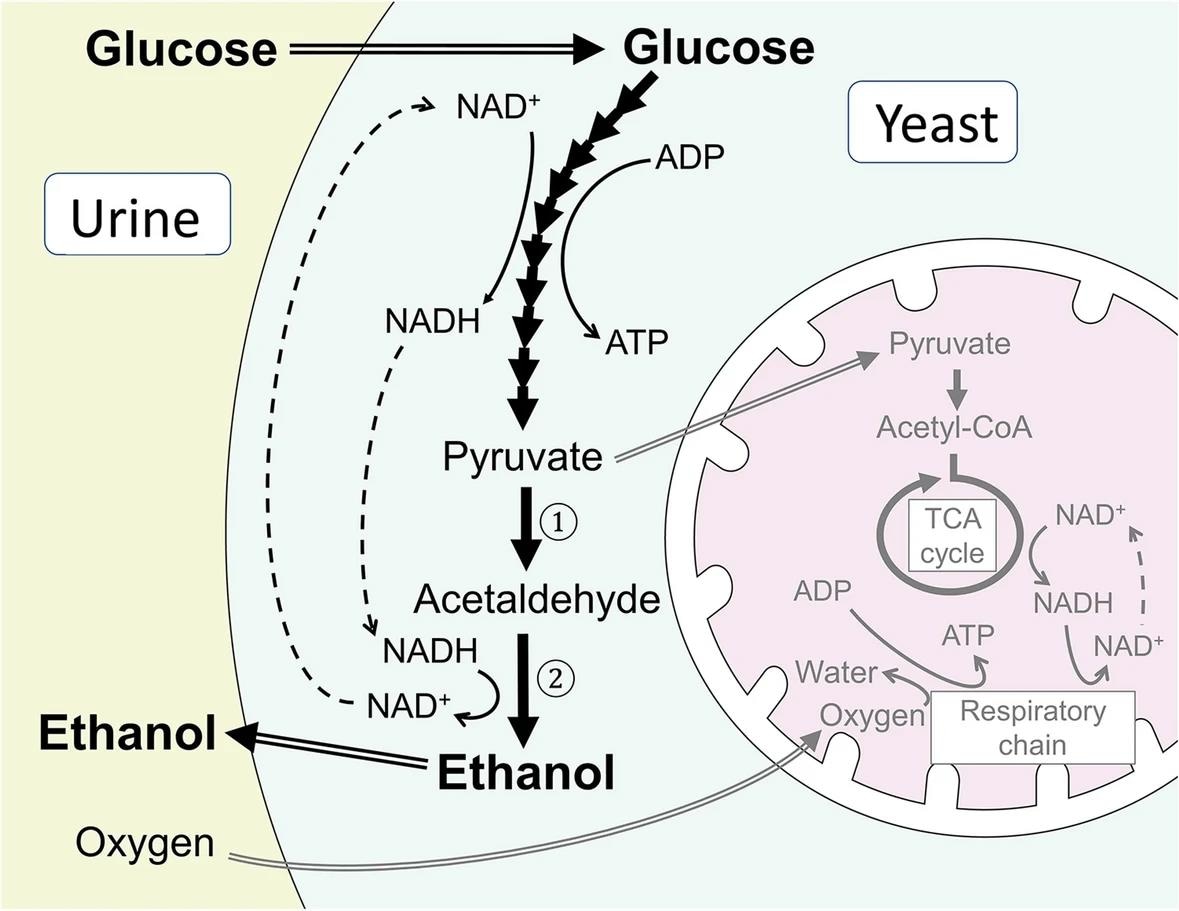
Simplified biochemical pathways illustrating glycolysis, alcoholic fermentation, and the TCA cycle in Crabtree-positive yeast. In Crabtree-positive yeast such as Candida glabrata, glucose is preferentially metabolized through glycolysis and alcoholic fermentation to ethanol in the cytosol without utilizing oxygen in the TCA cycle in mitochondria (shown in grey in the figure), even in the presence of oxygen in the surrounding environment as in the bladder lumen. In alcoholic fermentation, pyruvate is decarboxylated into acetaldehyde by pyruvate decarboxylase ①, and acetaldehyde is further metabolized to ethanol by alcohol dehydrogenase ②. TCA, tricarboxylic acid
BFS patients do not experience alcohol intoxication symptoms since their bladder wall's transitional epithelia operate as a low-permeability barrier for water and tiny molecules such as ethanol. Laboratory identification of yeast species and antifungal susceptibilities can aid in diagnosing and treating BFS. In BFS instances, ethanol metabolites are absent, requiring more precise experiments and test batterie to confirm the diagnosis.
BFS therapy entails managing hyperglycosuria and perhaps removing fermenting yeast from the bladder. Lowering urine glucose levels can slow fermentation and reduce the chance of establishing yeast colonies. Antidiabetic medications like dapagliflozin might increase glucose excretion and worsen BFS. Yeast colony elimination may require antifungal medications. However, S. cerevisiae and C. glabrata form biofilms that can impart resistance to the azole class of drugs. Monitoring alcohol abstinence is essential in addiction management, driver's license trials, driving under the influence (DUI) -type programs, and hepatic transplant assessments.
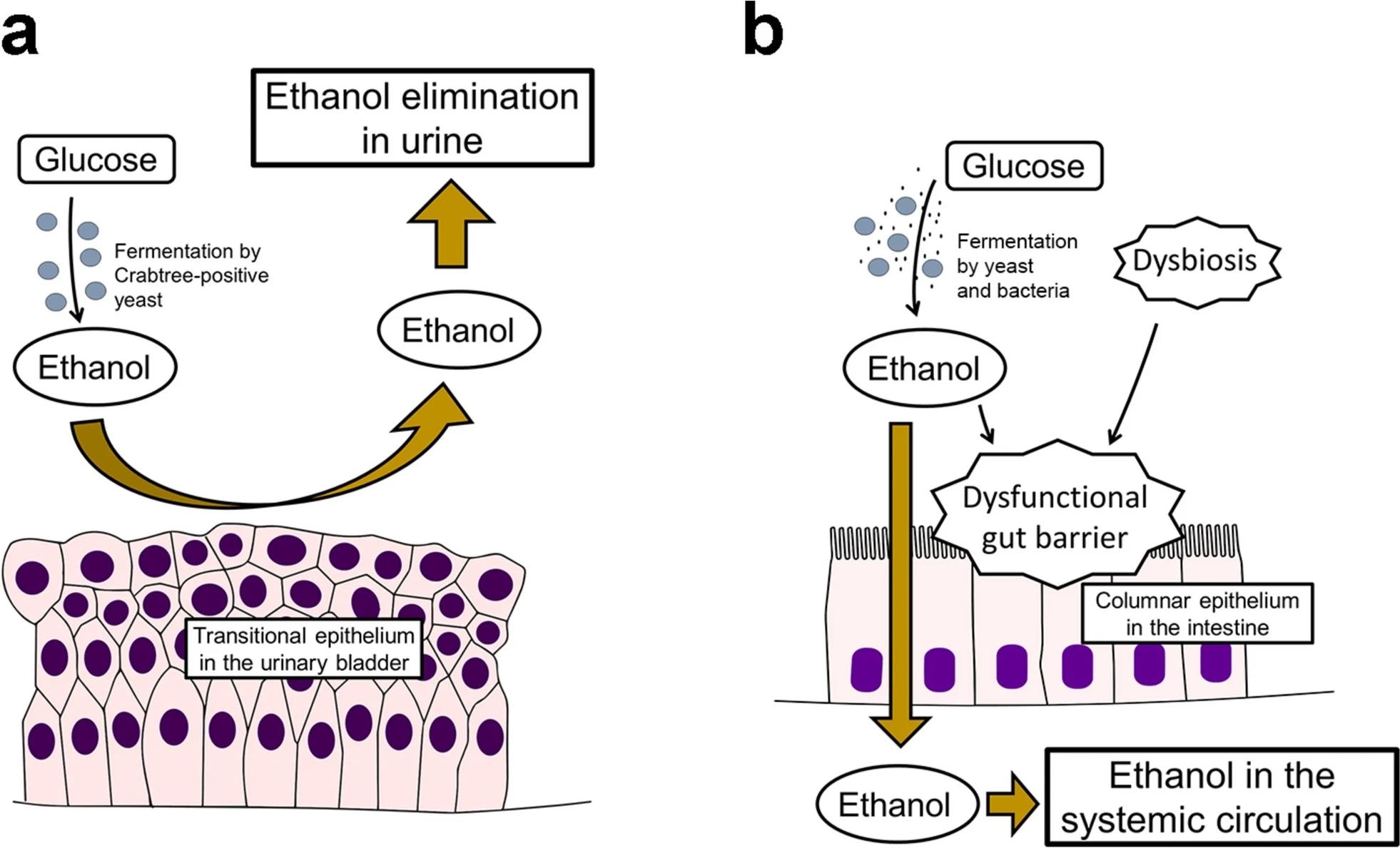 Pathophysiology of bladder fermentation syndrome and gut fermentation syndrome. a In bladder fermentation syndrome, ethanol produced through alcoholic fermentation by Crabtree-positive yeast is urinary-eliminated without getting absorbed into systemic circulation because the transitional epithelium in the urinary bladder serves as a barrier to ethanol. b In gut fermentation syndrome, ethanol produced through alcoholic fermentation by yeast and/or bacteria is absorbed into systemic circulation through the columnar epithelium in the intestine, causing alcohol intoxication. A dysfunctional gut barrier caused by dysbiosis and ethanol may also be involved in its pathogenesis
Pathophysiology of bladder fermentation syndrome and gut fermentation syndrome. a In bladder fermentation syndrome, ethanol produced through alcoholic fermentation by Crabtree-positive yeast is urinary-eliminated without getting absorbed into systemic circulation because the transitional epithelium in the urinary bladder serves as a barrier to ethanol. b In gut fermentation syndrome, ethanol produced through alcoholic fermentation by yeast and/or bacteria is absorbed into systemic circulation through the columnar epithelium in the intestine, causing alcohol intoxication. A dysfunctional gut barrier caused by dysbiosis and ethanol may also be involved in its pathogenesis
A comparison of BFS and GFS
GFS is an uncommon medical syndrome in which individuals experience symptoms of ethanol intoxication without having consumed alcohol. Alcoholic fermentation in the gut lumen causes GFS. GFS patients may fail abstinence regulation due to positive ethanol blood tests, putting them at risk for alcohol-related illnesses. GFS is similar to BFS, but it necessitates a thorough diagnostic evaluation and therapy, which includes a carbohydrate challenge test. Treatment consists of addressing underlying problems, removing fermenting bacteria, and adding carbohydrate-reduced diets and probiotics. Untreated BFS patients may develop repeated acute ethanol intoxication without drinking or spontaneous inebriation.
BFS and GFS are two different conditions defined by alcohol toxicity. Despite considerable ethanol levels in the urinary bladder, BFS patients do not show alcohol presence in their blood and do not exhibit intoxication symptoms, rendering them asymptomatic and unnoticed. GFS patients, on the other hand, might acquire alcohol intoxication without consuming any alcohol, which could result in legal implications like DUI. GFS sufferers may also fail abstinence testing and seek medical attention.
Disordered microbiota in hollow organs, resulting in ethanol fermentation by yeast in the stomach and bladder, cause BFS and GFS. Poorly managed diabetes, resulting in hyperglycosuria, often causes BFS. In contrast, GFS instances usually occur in individuals with underlying health conditions inducing gut microbial dysbiosis, like Crohn's disease, post-surgical short gut syndrome, and recent antibiotic usage. Fermenting yeast causes most GFS instances, although antifungal-resistant GFS associated with Klebsiella pneumoniae, a yeast that produces alcohol in large quantities, has occurred.
Based on the review findings, BFS and GFS are uncommon medical disorders frequently misconstrued due to their comparable etiology, clinical characteristics, and diagnostic testing. The under-recognition of these circumstances might lead to incorrect interpretations of abstinence monitoring, thereby preventing patients from getting medical therapy, such as transplantation. A primary cause of this underrecognition is a lack of scientific data on yeast and bacterial fermentation in the body. Future research should concentrate on determining the pathogenic functions of fermenting microbes in both illnesses, promoting awareness, and maybe clarifying terminology to improve medical professionals' comprehension.