Pain is a fundamental albeit unpleasant sensation that warns us of danger. It is increasingly clear that nerves can also have other functions, including signaling to epithelial cells that form the barrier of a tissue. We were inspired to see if pain fibers talk directly to epithelial cells in the gut to protect it from damage.
Dr. Yang and his co-author Dr. Jacobson discovered that the mucus lining of the gut was different when mice lacked pain fibers. This inspired the work that we carried out in this study. We wanted to really understand how pain regulates mucus levels and if this has consequences on gut tissue protection.
Daping Yang, Ph.D. - My Ph.D. training focused on Immunology, and I started my postdoctoral work in Chiu Lab three years ago. I am very interested in how the homeostasis of our gut mucosal barrier system is maintained and how this system senses and adapts itself to the ever-changing environment. As we all know, patients with inflammatory diseases usually suffer from visceral pain, which we also noticed in our mouse colitis model in the lab. However, whether pain, except for serving as an alert of danger, is involved in regulating gut barrier protection remains unknown.
 Image Credit: Lightspring/Shutterstock
Image Credit: Lightspring/Shutterstock
The presence of pain has been long recognized as an alert system, telling us to stop and pay attention to our bodies. Can you tell us more about pain itself, and how this alarm bell works to detect the potential presence of harm?
Pain is part of the body’s response to various noxious stimuli such as heat, chemical, or mechanical injuries. Pain is mediated by nociceptor neurons which have nerves present in the tissues. Nociceptor neurons express many receptors that allow them to quickly recognize and respond to those potentially damaging stimuli.
When the stimulation of nociceptor neurons goes above certain threshold, it will induce action potential that transduces the signal via the spinal cord to our brain, which makes us perceive pain and warns us about the presence of harm.
Your latest research suggests that on top of being an alert system, pain also plays a direct protective role in the gut, shielding it from damage. Can you tell us more about how you conducted your study?
To investigate the role of nociceptor neurons in the gut and host protection, we generated mice that lacked these pain-mediating neurons. As the mucus barrier is the first defense barrier of the gut mucosa, we first tried to measure the mucus layer thickness using immunostaining. We found that the mucus thickness was significantly decreased compared with that of the control group. With these results, we hypothesized that nociceptor neurons might be involved in mucus production. To confirm this, we also utilized a chemogenetic approach to activate the nociceptor neurons, which induced dramatically increased mucus thickness.
We next found the way neurons used a signal called CGRP to communicate with goblet cells, which are the cells that line our gut and produce mucus. This allows pain signaling to be coupled directly to mucus production. Gut microbes are one factor that causes neurons to produce CGRP and induce goblet cells to produce mucus. We also found that capsaicin, the ingredient in chili peppers found in spicy foods, also induced neurons to produce CGRP and induce mucus production by the gut. Finally, we also found that mice that lacked either nociceptor neurons or CGRP were more susceptible to colitis.
 Image Credit: Explode/Shutterstock
Image Credit: Explode/Shutterstock
Did the findings in mice match your expectations at the start of the study? What interesting results did you identify?
We were pretty open-minded about expectations at the start of our study. We did go into the study hypothesizing that pain and the neurons involved must play a more active role in regulating our gut barrier system. The most interesting result is our finding shows that goblet cells, the mucus-producing cells, highly express the receptor Ramp1, which recognizes neuropeptide CGRP secreted by nociceptor neurons.
These results suggest that nociceptor neurons might regulate goblet cell production through CGRP they produced. It also means mucus production is intimately associated with the nervous system. Another quite interesting finding is that the gut microbiome can regulate this process by stimulating nerves to release CGRP.
Your research discovered that intestinal goblet cells release protective mucus if triggered by direct interaction with the pain-sensing neurons within the gut. Can you tell us more about goblet cells in relation to the findings of your research?
Goblet cells are the key types of cells that produce and secrete mucus in the gut. Since the gut is a “mucosal” tissue, mucus is a fundamental part of the gut. On the one hand, it coats the gut and protects it from injury. On the other hand, it maintains a healthy microbiome that can feed on mucus-associated sugars, and also, mucus keeps a distance between harmful microbes and the gut wall.
We found that pain fibers can directly signal to goblet cells to regulate their function. In mice that lacked these pain-sensing neurons, the mucus lining is thinner, and this leads to microbial dysbiosis, meaning the community of gut microbes is not normal. It also made the mice more susceptible to colitis, which is inflammation in the colon. It is, therefore, important to understand how goblet cells receive signals from neurons and how this regulates their survival and function.
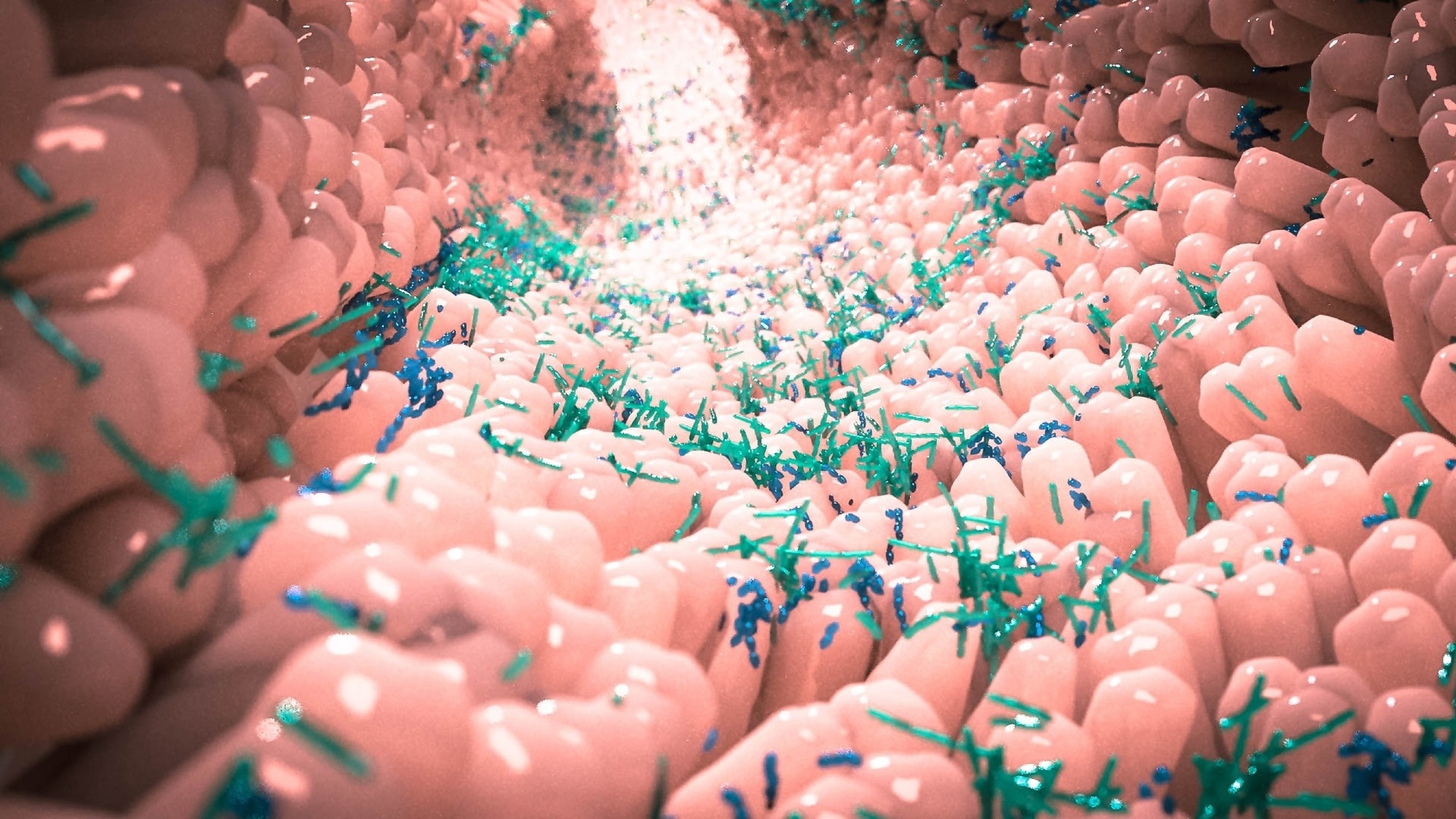 Image Credit: Alpha Tauri 3D Graphics/Shutterstock
Image Credit: Alpha Tauri 3D Graphics/Shutterstock
Your study also noted the possible downsides to suppressing pain. What are these downsides, and why is it so important to consider the possible consequences of blocking pain?
Because we found that pain protects the gut by mediating mucus production and maintaining a healthy microbiome, if we suppress pain, it could interfere with this protective property. There are people who have headaches and migraines who are currently taking drugs to block CGRP or its receptor RAMP1. Our findings suggest that blocking this pathway could lead to gut barrier problems, including mucus production and potentially also microbiome problems. It is already known that blocking CGRP can lead to constipation in the gut.
More broadly, beyond CGRP blockers, generally blocking pain signaling with opioids or other drugs could have unforeseen consequences on gut barrier function or mucus production that we should be cautious about.
What are the next steps for you to further your research?
We are very interested in further determining how neurons communicate with gut cells. We are, in particular, interested in how pain fibers talk to immune cells in the gut, which could have consequences on inflammation. Another very exciting question is defining how our microbiome affects pain fibers in the gut.
One of the implications of our research is that the microbiome signals, via these nerves, to regulate mucus levels. Therefore defining the products from microbes that act on pain fibers could be important.
Where can readers find more information?
Link to Chiu Lab: http://chiulab.med.harvard.edu
About the Interviewees:
Isaac Chiu, Ph.D. - Isaac Chiu is an Associate Professor in the Department of Immunology at Harvard Medical School. Dr. Chiu’s central research focus is neuro-immune interactions in pain, host defense and inflammation. He has found that nociceptor neurons directly detect bacteria and their mediators to produce pain. These neurons signal via neuropeptides to innate immune and epithelial cells in the skin and gut to mediate barrier immunity. Defining neuron-immune-microbe crosstalk could lead to new treatments for pain, infection, and inflammation.
and inflammation. He has found that nociceptor neurons directly detect bacteria and their mediators to produce pain. These neurons signal via neuropeptides to innate immune and epithelial cells in the skin and gut to mediate barrier immunity. Defining neuron-immune-microbe crosstalk could lead to new treatments for pain, infection, and inflammation.
Dr. Chiu received his Ph.D. in Immunology from Harvard Medical School in Mike Carroll’s lab and then did his postdoctoral training on the neurobiology of pain in Clifford Woolf’s lab at Boston Children’s Hospital. He started his independent faculty position at Harvard Medical School in 2014. Dr. Chiu has received the Burroughs Wellcome Fund Investigators in the Pathogenesis of Infectious Disease Award, NIH Director’s New Innovator Award, and Chan-Zuckerberg Initiative Ben Barres Award.
Daping Yang, Ph.D. - Daping Yang obtained his Ph.D. majoring in Immunology from the Shanghai Institutes for Biological Sciences of China, where he developed his research interest. He joined Professor Isaac Chiu's lab at Harvard Medical School as a postdoctoral student in 2020, aiming to understand the role of the gut-brain axis in gut mucosal barrier protection under homeostasis and inflammation. His current work focuses on how nociceptors and pain protect our gut health.