A woman in Maine developed a dangerous meat allergy after a black-legged tick bite—prompting the CDC to rethink which ticks can trigger alpha-gal syndrome. A decade of cases suggests the threat is broader than once believed.
 Dispatch: Alpha-Gal Syndrome after Ixodes scapularis Tick Bite and Statewide Surveillance, Maine, USA, 2014–2023. Image Credit: Aleksei Ruzhin / Shutterstock
Dispatch: Alpha-Gal Syndrome after Ixodes scapularis Tick Bite and Statewide Surveillance, Maine, USA, 2014–2023. Image Credit: Aleksei Ruzhin / Shutterstock
In a recent Dispatch published in the journal Emerging Infectious Diseases, researchers from the United States Centers for Disease Control and Prevention (CDC), the Maine Center for Disease Control and Prevention (Maine CDC), the University of North Carolina, and other institutions reviewed a case study from Maine to establish Ixodes scapularis as a potential carrier of alpha-gal syndrome (AGS). They retrospectively evaluated positive α-gal–specific IgE test results and case records collected over 10 years (2014–2023) as part of enhanced surveillance. They found that at least 23 Maine residents had similarly acquired the syndrome from unknown or potentially non-lone star tick exposures, highlighting the need for enhanced surveillance and medical attention to bites from other tick species.
Background
Alpha-gal syndrome, colloquially called the ‘mammalian meat allergy’ or the ‘tick bite meat allergy,’ is a severe allergic reaction (hypersensitivity) to the disaccharide galactose-α-1,3-galactose (α-gal) commonly found in mammalian meat products.
Symptoms include rash, hives, nausea or vomiting, difficulty breathing, drop in blood pressure, dizziness or faintness, diarrhea, severe stomach pain, and, in rare cases, anaphylaxis.
AGS is usually triggered following bites from the lone star tick, Amblyomma americanum, particularly in the United States of America. The syndrome's spatial distribution correlates strongly with the lone star tick's geographical distribution.
Notably, Ixodes holocyclus in Australia has also been implicated in triggering the condition, suggesting that bites from non-lone star tick species (e.g., Ixodes scapularis and Haemaphysalis longicornis) may be more worrisome than previously believed.
About the study
The present study investigates the case of a 45-year-old woman who depicted AGS-like symptoms following a bite from a non-lone star tick. The Maine Center for Disease Control and Prevention (Maine CDC) conducted the study.
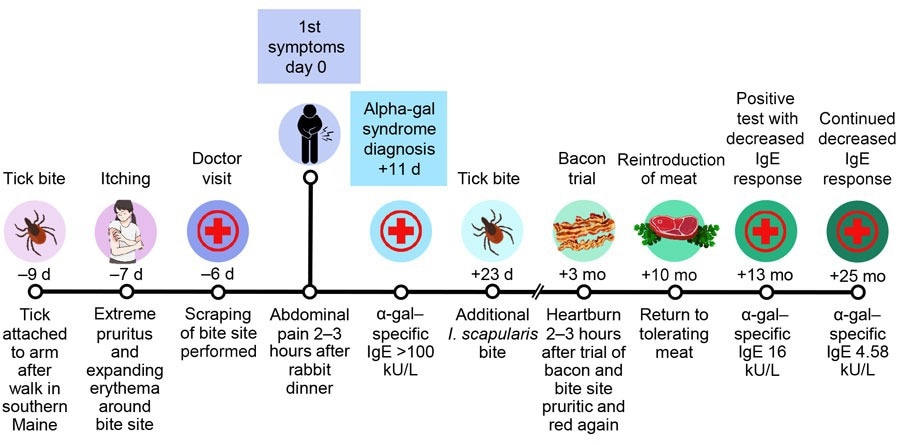
Timeline of symptom onset in a patient with alpha-gal syndrome after Ixodes scapularis tick bite, Maine, USA, 2022.
The study subject reported a tick bite (left bicep) received on the 4th of May 2022, discovered following her return from York County, Maine. The subject identified the tick as an adult female Ixodes scapularis, which was confirmed by the CDC using molecular and morphological data. Nine days later, in addition to the bite area demonstrating inflammation and severe itchiness, the subject reported delayed gastrointestinal (GI) symptoms (abdominal pain and malaise) following consumption of roasted rabbit.
These symptoms reoccurred frequently following the subject’s mammalian meal consumption over the following two weeks. Notably, the meals were shared, with only the subject reporting GI symptoms. Furthermore, the subject had no previous history of allergies or parasite exposure.
“A severe episode of diarrhea and vomiting hours after beef consumption prompted the patient to visit a healthcare provider (HCP) 20 days after the tick bite.”
Given her symptoms, her healthcare provider screened the subject through a panel of medical tests, including a metabolic panel, complete blood count, amylase, lipase, and Helicobacter pylori breath test. Simultaneously, an ultrasound (to detect gallstones) and a serum α-gal–specific IgE test were carried out. All tests demonstrated that the subject was in good health except the α-gal–specific IgE test, which was abnormally high (>100 kU/L).
Although she did not exhibit rash, hives, respiratory distress, or anaphylaxis, her symptoms were consistent with the gastrointestinal phenotype of AGS. Meal cofactors such as alcohol may have exacerbated symptom onset.
“Consumption of bacon at 3 months and steak at 7 months after first symptoms led to delayed heartburn sensations. Ten months after the first symptoms, the patient tolerated a steak dinner and roast beef sandwich and resumed eating red meat. α-gal–specific IgE at 13 months (June 13, 2023) measured 16 kU/L and at 25 months measured 4.58 kU/L.”
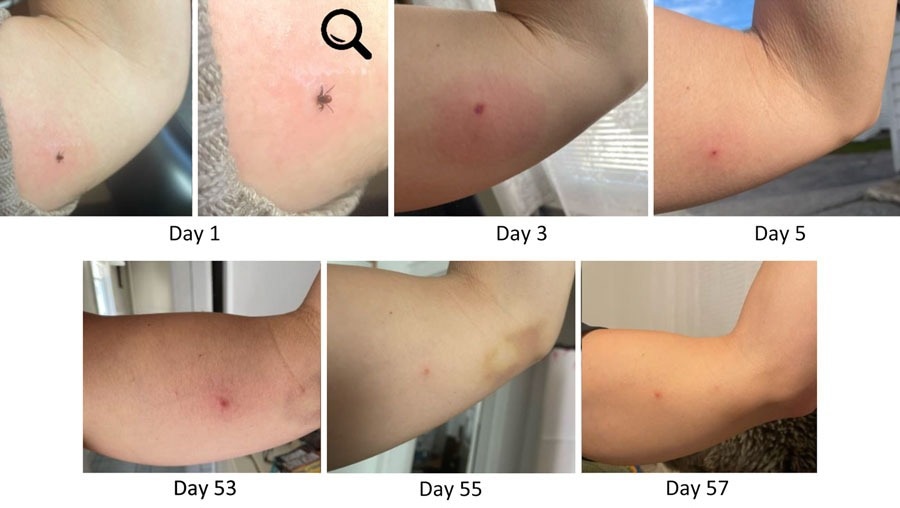
Progression and persistence of bite site reaction in alpha-gal syndrome after Ixodes scapularis tick bite, Maine, USA, 2022. A) Day 1, attached Ixodes scapularis adult female; B) enlarged version of image in panel A; magnification ×2.1; C) day 3, growing erythema surrounding tick bite site accompanied by intense and increasing pruritus; D) day 5, bite site less inflamed and with scab; E) day 53, patient resumed photo documentation because of persistent pruritus and “flares” of lesion becoming intermittently raised; F) day 55, lesion improved; G) day 57, lesion slightly raised again, photo taken to document variation. After these photos, pruritus largely resolved. As of December 2024, the bite site remains identifiable as an asymptomatic papule.
Study findings and follow-up
This case study provides evidence suggesting that bites from Ixodes scapularis can trigger hypersensitivity and AGS in humans. This, in turn, prompted the US CDC (Maine) to retrospectively collate and screen patient records from Maine spanning the 10 preceding years (2014–2023). Of the 57 Maine residents reporting AGS-like symptoms, IgE laboratory tests confirmed that 23 were positive for α-gal–specific allergies.
Interviews conducted with AGS confirmed cases and reviews of their travel history preceding their symptoms revealed contact with lone star, black-legged, and other ticks. However, the study acknowledges that not all tick exposures could be confirmed and that prior sensitization or multiple tick bites over a lifetime could contribute to AGS onset.
Conclusions
The present study suggests that non-lone star ticks, particularly the black-legged tick (Ixodes scapularis), may be implicated in AGS hypersensitivity in humans, greatly expanding the potential spatial distribution of the syndrome across the US.
To address this, the CDC has scaled up surveillance and advised clinicians and healthcare professionals to routinely screen tick bite patients for α-gal–specific IgEs.
Journal reference:
- Saunders EF, Sohail H, Myles DJ, Charnetzky D, Ayres BN, Nicholson WL, et al. Alpha-gal syndrome after Ixodes scapularis tick bite and statewide surveillance, Maine, USA, 2014–2023. Emerg Infect Dis. 2025, DOI – 10.3201/eid3104.241265, https://wwwnc.cdc.gov/eid/article/31/4/24-1265_article