Study findings surprisingly reveal that AUD patients seeking treatment for their condition and abstaining from alcohol consumption for at least six weeks presented the most distinct gut microbiota and metabolome composition, significantly higher in lipid super-pathway derived metabolites than the other two cohorts. Contrasting previous studies that noted improvements in gut microbial assemblages following alcohol abstinence, the current study highlights the potential long-term effects of alcohol abuse despite short-term absence. Furthermore, abstinence was found to be associated with substantially higher mental distress compared to currently drinking AUD participants.
What is AUD, and what do we know about it?
Alcohol Use Disorder (AUD) is a chronic behavioral condition characterized by uncontrolled alcohol consumption due to both emotional and physical dependence on the intoxicant. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) defines the condition as "a problematic pattern of alcohol use leading to clinically significant impairment or distress" and includes both binge drinking (>4 drinks in under 2 hours or blood alcohol concentrations exceeding 0.08%) and heavy drinking (>8 drinks per week) under the umbrella term.
Alarmingly, global AUD prevalence is on the rise, with an estimated mean prevalence of 5.1% worldwide and more than 10.2% in developed countries like the United States of America (US). AUD has been associated with a host of mental health conditions, particularly depression, socio-emotional impairment, psychosis, and anxiety disorders. The physical effects of prolonged alcohol consumption are also well documented and have been shown to include cancers, fetal alcohol syndrome, and, most recently, gut dysbiosis. Damage to the gut mucosal membrane results in increased gut permeability, which in extreme cases has been observed to release toxins into the circulatory system, ultimately severely damaging the liver.
Previous literature investigating the effects of abstinence in individuals seeking anti-AUD interventions has reported primarily positive outcomes, though study methodologies are often based on participant recall, confounding results.
"…including the failure to account for lifestyle and environmental factors known to affect gut bacteria contributing to intra- and inter-individual heterogeneity; in addition to retrospective measures of alcohol consumption which are subject to recall bias and strictly controlled inpatient settings, failure to properly account for these factors may deter researchers from making conclusive findings on whether gut dysbiosis and metabolic alterations are due to alcohol abstinence vs. factors intrinsic to inpatient care (e.g., diet, controlled environment) or other factors."
About the study
The present study aims to compare the gut microbiome and metabolome between three cohorts: 1. Abstinent individuals (AB, N = 10) comprised of AUD patients undergoing dependence interventions who had refrained from alcohol consumption for a minimum of 6 weeks; 2. Currently drinking individuals (CD, N = 9) consisting of DSM-5-confirmed AUD patients not undergoing interventions and consuming alcohol as usual, and 3. Healthy controls (HC, N = 12) who did not have a current or prior history of AUD and were age, sex, body mass index (BMI), and race matches to AB and CD cohort participants. Alcohol consumption was measured by the number of drinks per week (heavy drinking) or per two hours (binge drinking), where each drink was assumed to contain 14 g of alcohol.
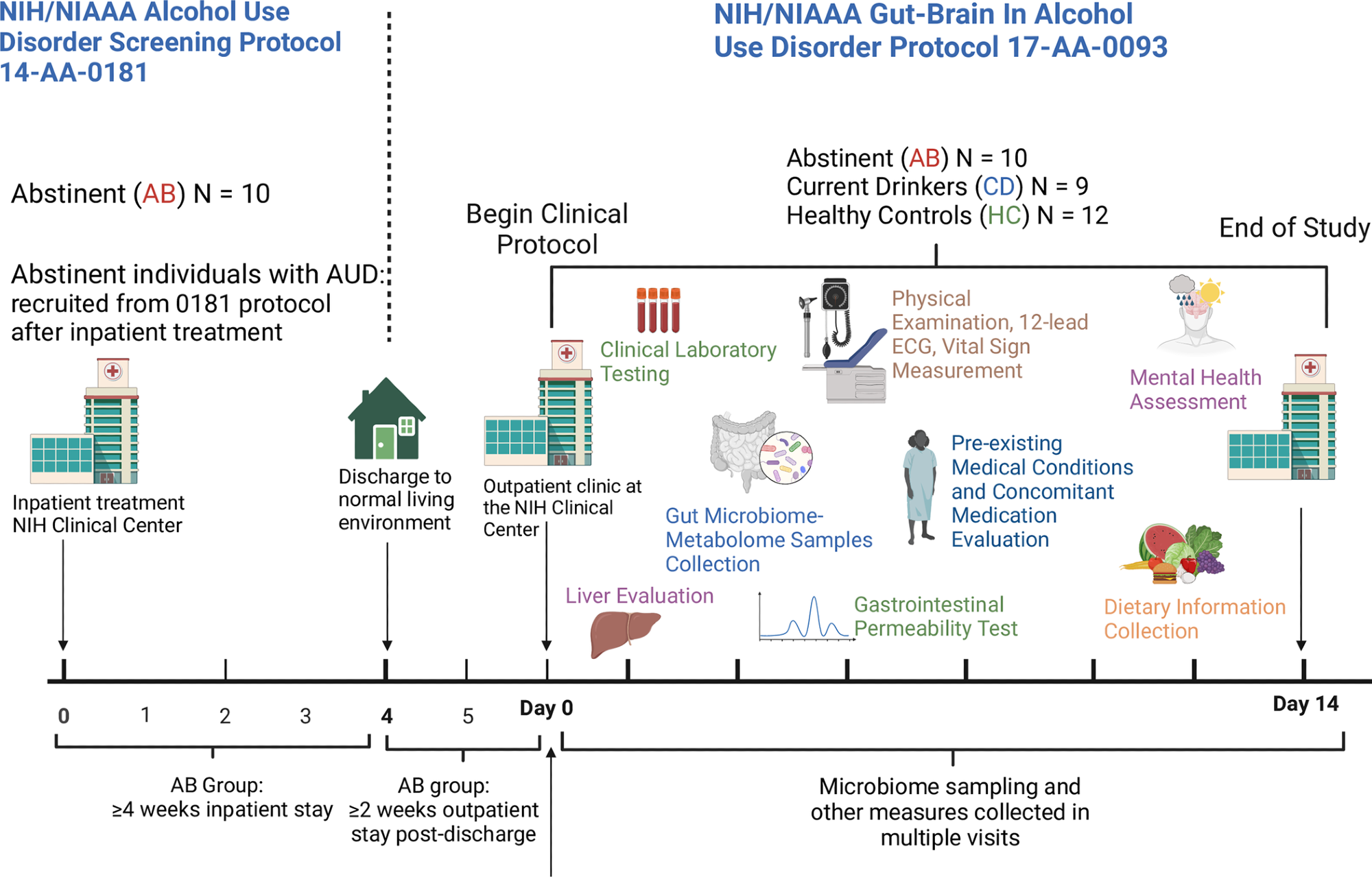
Schematic representation of the study design. Abstinent individuals with AUD (AB) were enrolled in the study after ≥4 weeks of inpatient treatment (NIH/NIAAA treatment protocol 14-AA-0181), followed by ≥2 weeks of “real life” (living their normal life). Non-treatment-seeking, currently drinking individuals with AUD (CD) and matched healthy controls (HC) were also enrolled. Fecal samples from the study participants were collected and processed for gut microbiome and metabolome analysis. Physical examination, 12-lead ECG, vital sign measurements, and laboratory tests were performed. Information on physical and mental health (including information on medical conditions and medications) and dietary intake was gathered and analyzed. Transient liver elastography and gastrointestinal permeability testing were carried out.
Data collection comprised participants' socioeconomic, demographic, and medical health records. Additionally, alcohol-associated clinical characteristics (e.g., AUD severity), mental health, and psychopathological features were evaluated both at the study baseline (in-person clinical assessment) and during frequent follow-up. Questionnaires, including the Penn Alcohol Craving Scale (PACS), Clinical Institute Withdrawal Assessment of Alcohol Scale, Revised (CIWA-Ar), and the Alcohol Use Disorders Identification Test (AUDIT), were used to collate participant-provided data.
Liver transient elastography was used to identify and diagnose liver steatosis and fibrosis. Gastrointestinal permeability testing was carried out to evaluate gut mucosal integrity. Fecal samples (collected at study initiation and again at final follow-up) were used for microbiome and metabolome analyses, the former of which was conducted via 16S rRNA sequencing.
Study findings and conclusions
Contrasting previous studies and the researchers' hypothesis, the results of the present study not only revealed that short-term alcohol abstinence among former AUD patients does not improve their gut microbial health, but it also instead displays substantial gut dysbiosis, exceeding that of current AUD patients who continue to drink normally. AB cohort individuals were additionally found to experience increased anxiety and depression and lower sleep quality than either CD or HC, albeit the underlying cause of these results could not be differentiated between alcohol withdrawal or a physical consequence of sudden abstinence.
"…we hypothesized gut microbiome/metabolome similarities between healthy controls and newly abstinent individuals with AUD, while the CD group was going to be different than the other two groups. By contrast, it was the AB group to separate itself, from a gut microbiome/metabolome standpoint, from the other two groups."
Gut microbiome and metabolome analyses revealed that AD cohort individuals experienced depletions of beneficial microbial populations (such as Akkermansia, Lachnospira, Roseburia, Fusicatenibacter, and Lachnospiraceae_UCG_001) compared to CD and HC participants in whom abundances of these gut flora were more or less consistent. Similarly, both uni- and multivariate analyses revealed AB's fecal metabolomes to differ significantly from the other two groups in at least 33 identified metabolites, all primarily associated with lipid and amino acid pathways.
"Consistent with the conclusions above, AB group reported being affected by significantly more medical conditions and therefore taking significantly more medications than the other groups. These findings imply that gut microbiome and metabolome differences observed in AB individuals compared to CDs and HCs may therefore be due to a higher prevalence of diseases and a higher intake of medications in the AB group."
In summary, the present work highlights that short-term abstinence from prolonged heavy or binge drinking may exacerbate the adverse long-term effects of AUD rather than reversing them. Further research is required to confirm if long-term abstinence can result in gradual or eventual recovery from these adverse effects, but given presently available information, breaking the bad habit (herein frequent or excessive alcohol consumption) before it becomes an addiction is the best course of action.
Journal reference:
- Piacentino, D., Vizioli, C., Barb, J. J., Grant-Beurmann, S., Bouhlal, S., Battista, J. T., Jennings, O., Lee, M. R., Schwandt, M. L., Walter, P., Henderson, W. A., Chen, K., Turner, S., Yang, S., Fraser, C. M., Farinelli, L. A., Farokhnia, M., & Leggio, L. (2024). Gut microbial diversity and functional characterization in people with alcohol use disorder: A case-control study. In J. J. Loor (Ed.), PLOS ONE (Vol. 19, Issue 6, p. e0302195). Public Library of Science (PLoS), DOI – 10.1371/journal.pone.0302195, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0302195