In a recent study published in the journal JACC Advances, researchers in the United States examined the presence of coronary atherosclerosis using coronary computed tomography angiography (CCTA) in asymptomatic adults without traditional risk factors based on their serum levels of low-density lipoprotein cholesterol (LDL-C), non-high-density lipoprotein cholesterol (non-HDL-C), and apolipoprotein B (apoB). They found that coronary atherosclerosis is common, and the prevalence increases with increasing levels of atherogenic lipoproteins, even in low-risk adults without traditional risk factors.
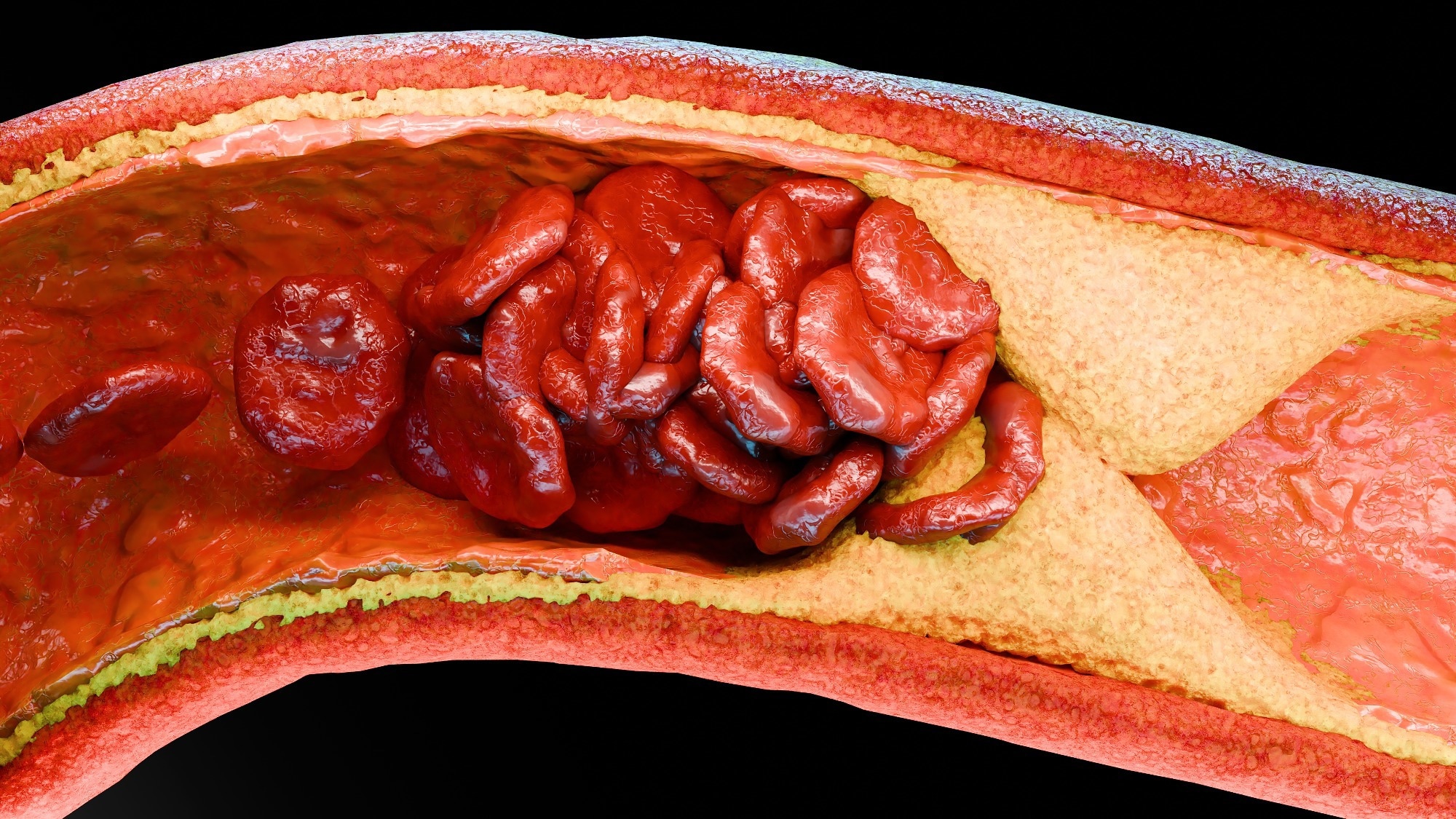 Study: Serum Lipoproteins Are Associated With Coronary Atherosclerosis in Asymptomatic U.S. Adults Without Traditional Risk Factors. Image Credit: ALIOUI MA / Shutterstock
Study: Serum Lipoproteins Are Associated With Coronary Atherosclerosis in Asymptomatic U.S. Adults Without Traditional Risk Factors. Image Credit: ALIOUI MA / Shutterstock
Background
Atherosclerotic cardiovascular disease (ASCVD) is a major cause of mortality globally, mainly owing to coronary atherosclerosis, which is known to have an early onset and shows progression over time. Increased LDL-C is a significant cause of ASCVD, and lowering LDL-C is crucial for prevention. Historically, LDL-C ≥160 mg/dL was considered elevated, while <100 mg/dL was deemed optimal. However, these levels may still be insufficient to prevent atherosclerosis or ASCVD. Additionally, non-HDL-C and apoB are strong predictors of ASCVD but are rarely evaluated in asymptomatic populations. There remains a dearth of evidence on the relationship between these lipoproteins and coronary atherosclerosis in adults lacking clinical ASCVD or other risk factors. Therefore, researchers in the present study investigated the association between subclinical coronary atherosclerosis and atherogenic lipoproteins in asymptomatic, middle-aged US adults lacking traditional ASCVD risk factors. They hypothesized a potentially significant correlation and aimed to enhance the primary diagnostic and prevention strategies employed against the condition.
About the study
The present study's data were sourced from the Miami Heart (MiHeart) study. A total of 1,033 participants were included from the age group 40–65 years and free of clinically symptomatic cardiovascular disease or lipid-lowering therapy, with a subgroup of 184 participants having optimal risk factors. Individuals with high-risk conditions, such as obesity, high creatinine levels, asthma, cancer, or pregnancy, were also excluded. The median age of the participants was 51 years, 42.1% of them were non-Hispanic White, and 55% were female. Data on demographics, clinical history, and CCTA imaging were obtained. Coronary atherosclerosis was diagnosed using the Agatson method and the American Heart Association classification. The study examined the potential association of non-HDL-C, LDL-C, and apoB with coronary atherosclerosis, significant stenosis, coronary artery calcification, and high-risk plaque features. The statistical analysis involved the use of t-tests, chi-square tests, Fisher's exact tests, and logistic regression models with forward stepwise selection.
Results and discussion
The study cohort had median serum LDL-C, non-HDL-C, and apoB levels of 125, 144, and 94 mg/dL, respectively. A majority of the participants had a lower predicted 10-year ASCVD risk, with over 86% having <5% risk. Men showed a higher body mass index, atherogenic lipoprotein levels, and ASCVD risk compared to women. About 35.9% of participants without traditional ASCVD risk factors had coronary plaque, and the prevalence of coronary and calcified plaque was found to increase progressively with the levels of non-HDL-C, LDL-C, and apoB. Men showed higher plaque rates and more high-risk features than women. Further, coronary plaque was observed to become more common with advancing age in both men and women. Multivariable analyses showed that higher atherogenic lipoproteins, age, male sex, and high lipoprotein(a) were significantly associated with coronary plaque.
In the optimal risk factor subgroup, 21.2% had coronary plaque but less frequently had severe or high-risk plaque features. Increased age and male sex were observed to be the key predictors of coronary atherosclerosis. At the same time, higher levels of non-HDL-C, LDL-C, and apoB were found to remain positively associated with coronary plaque. However, these associations were not statistically significant in this smaller group.
The study is strengthened by its large, community-based cohort of asymptomatic adults, detailed assessment of both noncalcified and calcified coronary plaque using CCTA, and its focus on a broad range of atherogenic lipoproteins and high-risk plaque features. However, the study is limited by its single-time-point data collection, lack of dietary and activity information, a potentially underpowered optimal risk factor subgroup, non-representative sample, and the absence of longitudinal clinical outcomes.
Conclusion
In conclusion, the study suggests that among asymptomatic, apparently healthy, middle-aged US adults without traditional ASCVD risk factors, coronary atherosclerosis is common even at serum cholesterol levels considered to be normal. The condition's prevalence increases with higher LDL-C, non-HDL-C, and apoB. Despite this population's relatively infrequent high-risk plaque features, healthcare professionals should consider lowering serum atherogenic lipoproteins through diet, lifestyle changes, or medication to potentially prevent or delay coronary atherosclerosis and improve their health outcomes. In the future, studies could focus on the best timing for risk assessment, the role of supplemental imaging, and the use of lipid-lowering therapy in low-risk adults.