SARS-CoV-2 typically causes mild illness in children but can lead to MIS-C, a rare, life-threatening condition. This condition presents with a complex and heterogeneous clinical profile, making it particularly challenging to understand. MIS-C is characterized by a distinct inflammatory signature indicative of altered innate immunity. In particular, dysregulation of the mitochondrial antiviral signaling (MAVS) protein pathway has been highlighted in MIS-C pathology, contributing to the unique inflammatory profile observed in these patients. Besides, aberrant adaptive immunity is also involved. Various MIS-C-associated autoantibodies have been reported. Further, T cell signatures are also associated with MIS-C development, accompanied by autoimmune-related B cell expansions. However, pathological links between SARS-CoV-2 and MIS-C are unclear.
The study’s rigorous design involved comprehensive evaluations of proteome-wide autoantibody profiles, leveraging a larger cohort size than previous studies to ensure robustness and minimize spurious associations.
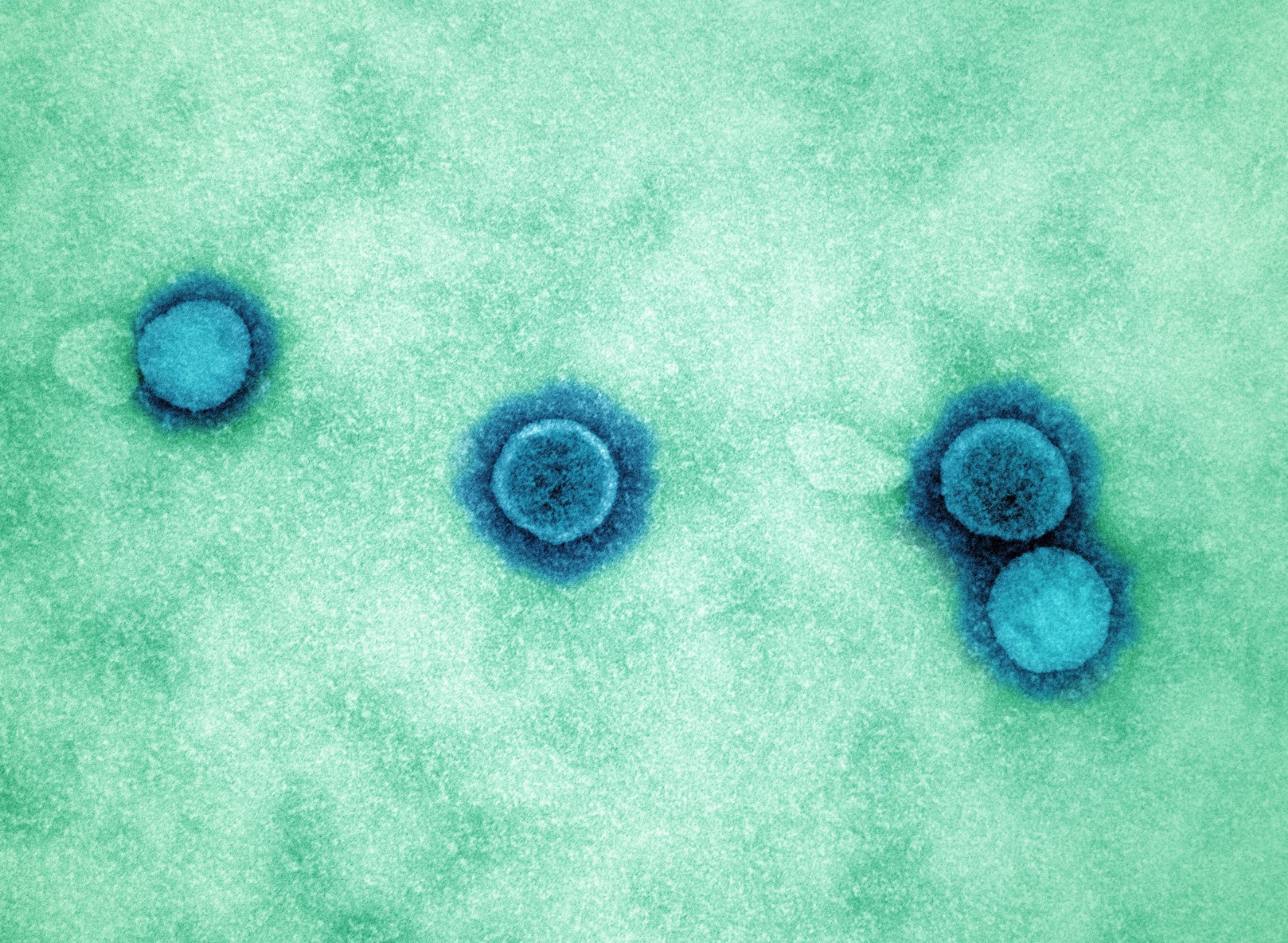 Study: Molecular mimicry in multisystem inflammatory syndrome in children. Image Credit: NIAID
Study: Molecular mimicry in multisystem inflammatory syndrome in children. Image Credit: NIAID
The study and findings
The present study evaluated differential autoreactivity to SARS-CoV-2 and human proteomes in SARS-CoV-2-infected children with and without MIS-C. Patients were recruited from the “Overcoming COVID-19 and Taking on COVID-19 Together” study, involving a detailed analysis of clinical characteristics to correlate with proteomic findings. Plasma samples from healthy pre-COVID-19 controls were obtained from a blood center.
First, the team used a customized phage immunoprecipitation and sequencing (PhIP-seq) library to analyze autoantibody profiles of 199 children with MIS-C and 45 at-risk controls (those convalescing post-infection without MIS-C). This approach has previously been validated in identifying novel autoimmune markers across various conditions, providing a strong foundation for this study’s methodology. Logistic regression was used to measure the accuracy of differential peptide enrichments to classify MIS-C patients and controls.
Overall, 107 proteins (classifier set) had regression coefficients > 0. This classifier set was further refined using a Kolmogorov–Smirnov test to ensure statistical significance, resulting in a highly selective group of candidate autoantigens. The receiver operating characteristic curve was generated for the classifier set and iterated 1,000 times. The area under the curve was 0.94, on average. Analysis of the MIS-C-associated regression coefficients revealed the highest contributions from KDEL endoplasmic reticulum protein retention receptor 1 (KDELR1), sorting nexin 8 (SNX8), and ETS repressor factor-like (ERFL) peptides.
While 34 autoantigens have been previously reported to be associated with MIS-C, only ubiquitin-protein ligase E3A (UBE3A) was differentially enriched in this dataset. Interestingly, while UBE3A was the only previously reported autoantigen to be confirmed, the study’s larger cohort and refined methods underscore the need for re-evaluation of earlier findings in MIS-C autoimmunity. Antibodies against interleukin 1 (IL-1) receptor antagonist (IL-1RA) were detected in six patient samples. Further, sera from 196 patients were used to immunoprecipitate radiolabeled IL-1RA by a radioligand-binding assay (RLBA).
Around 20% of samples had positive IL-1RA immunoprecipitation. This finding raises important questions about the role of IVIG treatment in MIS-C, as many patients in this study had received IVIG, which is known to contain autoantibodies. Most MIS-C patients received intravenous immunoglobulin (IVIG), which contains autoantibodies. As such, after removing IVIG-treated samples, the difference between MIS-C cases and at-risk controls was insignificant. Further, RLBAs were performed to orthogonally validate PhIP-seq findings using full-length KDELR1, SNX8, and ERFL.
MIS-C patient samples were significantly enriched for these proteins compared to at-risk controls. This enrichment was validated in an independent cohort, further solidifying the diagnostic potential of these proteins. MIS-C could be classified from at-risk controls using only RLBA data of the three proteins, suggesting diagnostic potential. Unlike IL-1RA, after removing IVIG-treated samples, the differential enrichment of the three proteins was significant.
Furthermore, the team validated these findings in an independent cohort of 24 MIS-C cases with severe acute coronavirus disease 2019 (COVID-19), suggesting that autoreactivity to the three proteins is a characteristic of MIS-C, distinct from exposure to SARS-CoV-2. This distinction is crucial, as it highlights the unique immunopathology of MIS-C beyond mere SARS-CoV-2 exposure. Next, SNX8 was selected for further analysis, given its putative role in the mitochondrial antiviral signaling (MAVS) pathway in RNA virus infections and enrichment in immune cells.
In the PhIP-seq assay, a peptide fragment of SNX8 spanning amino acids 25–73 was the most enriched in all patients except one. A sequential alanine scan of six MIS-C samples identified a nonamer (amino acids 51-59) as the critical immunoreactive region. Further, immunoreactivity against a wild-type fragment and version mutated to alanine was assessed.
Thirty-one patient samples immunoprecipitated with the wild-type fragment; of these, 29 did not immunoprecipitate with the mutated fragment, suggesting a common autoreactive epitope in MIS-C patients with anti-SNX8 antibodies. This finding suggests a precise immunoreactive motif that may play a central role in the autoimmune aspect of MIS-C. Next, the team repeated PhIP-seq using a custom SARS-CoV-2 library. There was significant enrichment of three peptides (fragments 5, 8, and 9) derived from the viral nucleocapsid.
Fragment 5 was enriched in at-risk controls, while the other two (8 and 9) were enriched in MIS-C patients. Fragment 8 was the most differentially reactive in patients and was thus deemed the MIS-C-associated domain of SARS-CoV-2 (MADS). Moreover, the critical immunoreactive region in MADS and SNX8 was highly similar and represented by (ML)Q(ML)PQG. This sequence similarity supports the hypothesis of molecular mimicry as a driver of MIS-C, potentially explaining the cross-reactive immune responses observed in patients.
Next, the team tested whether MIS-C patients with anti-SNX8 antibodies have autoreactive T cells against SNX8-expressing cells. Seven MIS-C patients had autoreactive T cells against SNX8-expressing cells, but none of the at-risk controls possessed autoreactive T cells. In addition, MIS-C patients also had T cells cross-reactive to MADS and SNX8 similarity regions. These T cells may play a pivotal role in the pathogenesis of MIS-C by inappropriately targeting immune cells expressing SNX8, leading to immune dysregulation.
Conclusions
The study analyzed samples from MIS-C patients and at-risk controls using custom SARS-CoV-2 and human PhIP-seq proteome libraries. The comprehensive nature of this analysis, involving multiple cohorts and rigorous validation, adds significant weight to the findings. The findings revealed that MIS-C patients preferentially harbored antibodies against the epitope motif (ML)Q(ML)PQG, shared by the human SNX8 protein and SARS-CoV-2 nucleocapsid.
Moreover, cross-reactive T cells targeting the epitope were detected in MIS-C patients but not in controls. This dual reactivity of both B and T cells highlights a critical mechanism of immune dysregulation in MIS-C, suggesting that these cross-reactive T cells may be key players in the disease process. This suggests that these T cells may contribute to immune dysregulation by inappropriately targeting SNX8-expressing immune cells. Besides, the epitope elicited both T and B cell reactivity, warranting further analysis of epitope convergence.
This dual reactivity of both B and T cells highlights a critical mechanism of immune dysregulation in MIS-C, suggesting that these cross-reactive T cells may be key players in the disease process.